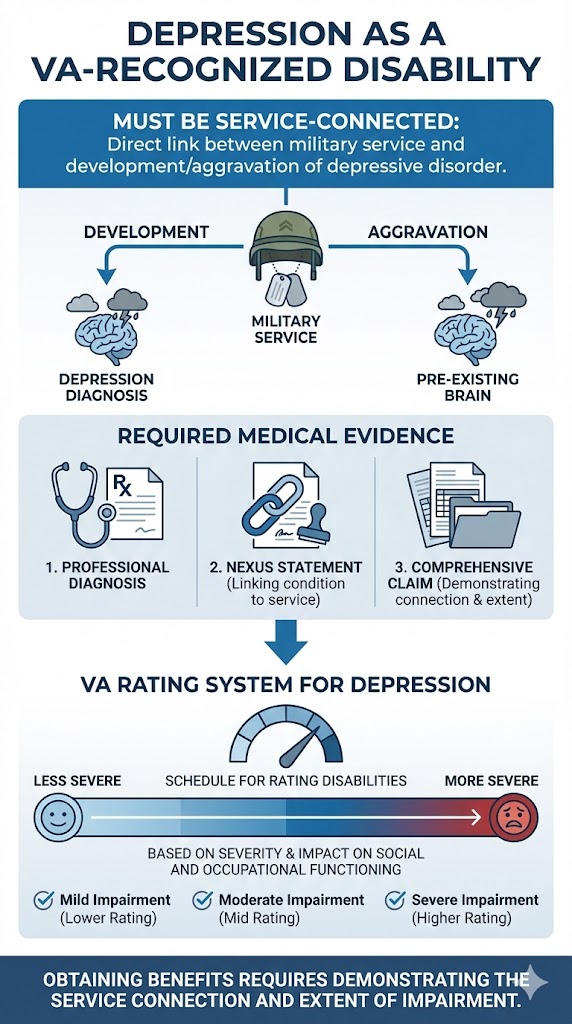
Yes, depression can be recognized as a disability by the Department of Veterans Affairs (VA) if it is service-connected. This means there must be a direct link between your military service and the development or aggravation of your depressive disorder. Veterans must provide medical evidence, including a diagnosis from a qualified professional and a nexus statement linking the condition to service. The VA rates depression based on its severity and impact on social and occupational functioning, using the Schedule for Rating Disabilities. Obtaining benefits requires a comprehensive claim demonstrating the service connection and the extent of impairment.
Understanding Depression as a Recognized Disability
Depression is a mental health condition characterized by persistent sadness, loss of interest, and other symptoms that can significantly affect daily life. Under Americans with Disabilities Act (ADA) laws, depression may be considered a disability if it substantially limits one or more major life activities. This legal recognition extends beyond the workplace and applies to various aspects of civilian life.
For veterans, the VA recognizes depressive disorders as potentially compensable conditions if service-connected. A diagnosis from a qualified mental health professional is the first step in recognizing depression as a medical condition for disability purposes. This diagnosis forms the foundation of your claim and helps establish the severity of your condition.
Establishing Service Connection for VA Disability Benefits
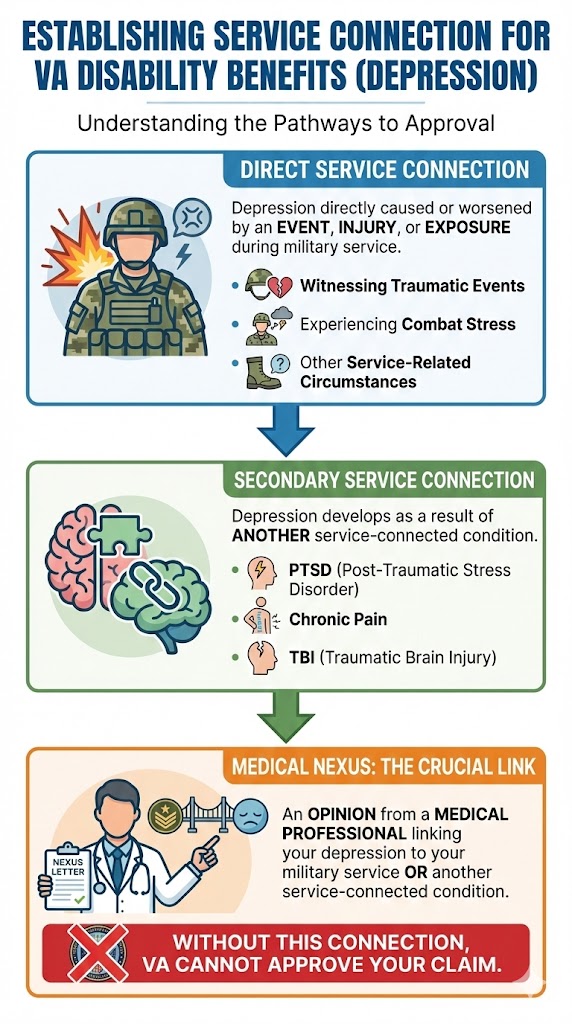
Direct Service Connection occurs when depression is directly caused or worsened by an event, injury, or exposure during military service. This could include witnessing traumatic events, experiencing combat stress, or enduring other service-related circumstances that led to the development of your depressive disorder.
Secondary Service Connection happens when depression develops as a result of another service-connected condition, such as PTSD (Post-Traumatic Stress Disorder), chronic pain, or TBI (Traumatic Brain Injury). This is a common pathway for depression claims, as many physical and mental health conditions can contribute to the development of depressive symptoms over time.
A medical nexus (medical link) is important for establishing service connection. This is an opinion from a medical professional linking your depression to your military service or another service-connected condition. Without this connection, the VA cannot approve your claim for benefits.
How the VA Rates Depressive Disorders
According to 38 CFR § 4.130 (the federal regulation governing VA mental health ratings), the VA rates depressive disorders, including their dysthymic and cyclothymic presentations, under Diagnostic Code 9434 within the Schedule for Rating Disabilities, Mental Disorders section. This diagnostic code provides the framework for evaluating the severity of your condition and assigning an appropriate disability rating.
Ratings range from 0% to 100% in increments of 10%, 30%, 50%, 70%, and 100%, based on the severity of symptoms and the resulting social and occupational impairment. The VA examines how your depression affects your ability to work, maintain relationships, and perform daily activities when determining your rating percentage.
Factors considered include the frequency and duration of psychiatric hospitalization, inability to perform work, and extent of impairment in social relationships and daily self-care. A C&P examination (Compensation and Pension examination) by a VA-appointed medical professional is an important part of the rating process, assessing current symptoms and their impact on your functioning.
Key Evidence Required for a Successful Claim
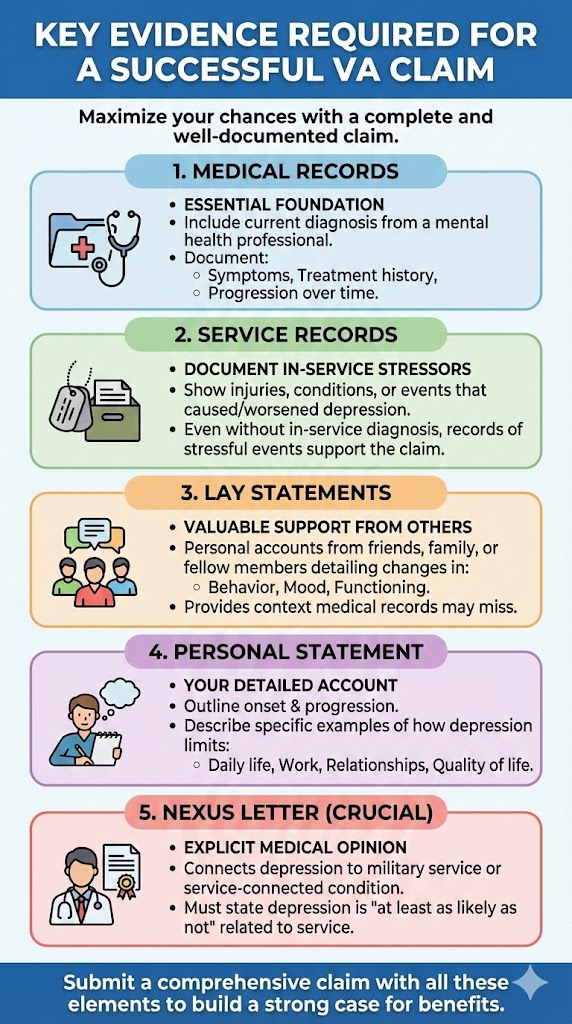
Medical Records are essential and should include a current diagnosis of depression from a psychiatrist, psychologist, or other mental health professional. These records should document your symptoms, treatment history, and the progression of your condition over time.
Service Records provide documentation of in-service stressors, injuries, or conditions that could have led to or worsened your depression. Even if you weren’t diagnosed during service, records showing stressful events or circumstances can support your claim.
Lay Statements from friends, family, or fellow service members can provide valuable support for your claim. These personal accounts detail changes in behavior, mood, and functioning observed before, during, and after service, providing context that medical records alone cannot capture.
Personal Statement is your own detailed account of how depression affects your daily life, work, and relationships. You should outline the onset and progression of symptoms, describing specific examples of how your condition limits your activities and affects your quality of life.
Nexus Letter is a medical opinion from a doctor that explicitly connects your depression to your military service or an existing service-connected condition. This letter should state that your depression is “at least as likely as not” related to your service.
Navigating Challenges in the VA Claims Process
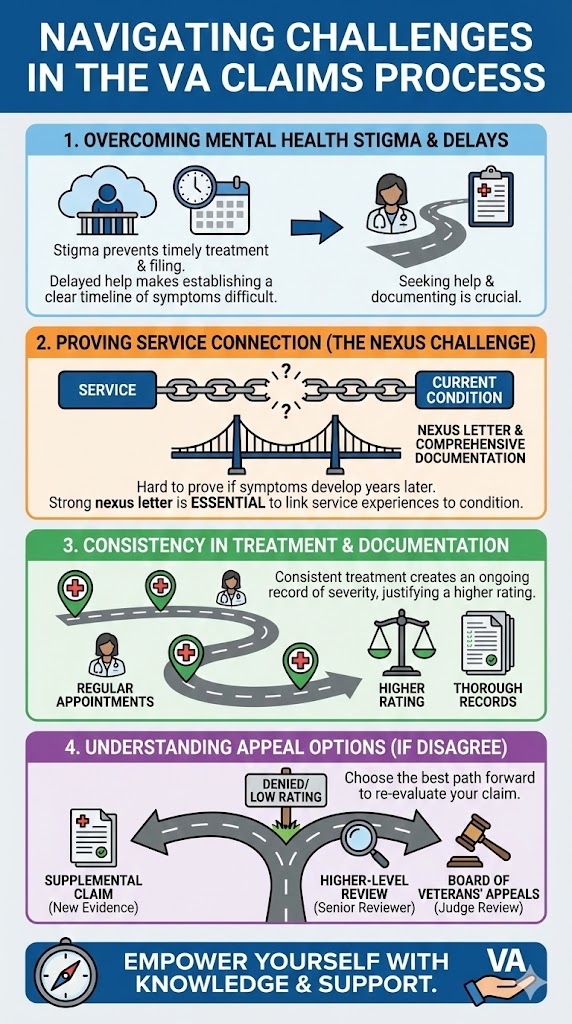
The stigma associated with mental health conditions may prevent some veterans from seeking timely treatment or filing claims, which can complicate evidence gathering. Many veterans delay seeking help, making it harder to establish a clear timeline of symptoms and their connection to service. This delay is understandable given the challenges of seeking mental health support.
Proving a direct service connection can be challenging, especially if symptoms developed years after separation. This emphasizes the need for a strong nexus letter and comprehensive documentation showing the link between your service experiences and your current condition.
Consistency in treatment and thorough documentation of symptoms and their impact are important for supporting a claim and justifying a higher rating. Regular mental health appointments create a treatment record that demonstrates the ongoing nature and severity of your depression.
If you disagree with a VA decision, you have three main appeal options: filing a Supplemental Claim, requesting a Higher-Level Review, or appealing to the Board of Veterans’ Appeals. Each option allows for different approaches to re-evaluating your claim. Understanding these options helps you choose the best path forward if your initial claim is denied or you receive a lower rating than expected.
Example Scenario
An Army veteran, began experiencing depression, including anhedonia (loss of interest or pleasure) and social isolation, two years after her deployment where she witnessed traumatic events. Although she didn’t have an in-service diagnosis, her therapist provided a comprehensive medical report and a strong nexus letter, clearly linking her current depressive disorder to her military service.
She also submitted lay statements from her spouse and friends detailing her changes in personality and behavior after service. These statements, combined with her medical evidence, helped her secure a VA disability rating for her depression.
Frequently Asked Questions
Can depression alone qualify for 100% VA disability?
Yes, if the severity of symptoms for depression is so profound that it results in total social and occupational impairment, it can qualify for a 100% VA disability rating. This means the veteran is unable to work or maintain social relationships due to their condition.
What is a ‘nexus letter’ and why is it important for a depression claim?
A nexus letter is a medical opinion from a qualified healthcare provider stating that your depression is ‘at least as likely as not’ caused by or aggravated by your military service. It is critical for establishing service connection, especially if there isn’t clear evidence of the condition in your service records.
Do I need an in-service diagnosis of depression to get VA benefits?
No, an in-service diagnosis is not strictly required. While helpful, you can still establish service connection with a current diagnosis and a strong medical nexus linking your post-service depression to an event, injury, or condition that occurred during your military service.
How long does it take for the VA to decide a depression claim?
The timeline for a VA claim decision varies significantly. It depends on factors like the complexity of the claim, the completeness of evidence, and the VA’s current workload. Decisions can range from several months to over a year or more.
Can I claim depression secondary to another service-connected condition like PTSD or chronic pain?
Yes, depression is frequently claimed as secondary to other service-connected conditions, such as Post-Traumatic Stress Disorder (PTSD), Traumatic Brain Injury (TBI), or chronic physical pain. This is because these conditions can significantly contribute to the development or worsening of depressive symptoms.
What is the difference between depression and PTSD for VA purposes?
While both are mental health conditions rated under the same diagnostic schedule, PTSD specifically arises from exposure to a traumatic event and has distinct diagnostic criteria (e.g., re-experiencing, avoidance, hyperarousal). Depression is a broader mood disorder characterized by persistent low mood and loss of interest, though symptoms can overlap. Both can be service-connected.
What kind of medical evidence does the VA look for when evaluating depression?
The VA primarily looks for a formal diagnosis of depression from a qualified mental health professional, detailed treatment records, notes on symptom severity and frequency, and how these symptoms impact your social, occupational, and personal life. Information from your Compensation and Pension (C&P) exam is also important for the evaluation process.
If you want more help with your benefits, contact us here at AllVeteran.com! You can take our free medical evidence screening to get help with understanding your options.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.