Dysphagia, or difficulty swallowing, is a condition for which veterans can receive VA disability benefits. The VA rates dysphagia under Diagnostic Code 7203 (stricture of the esophagus) within the Schedule of Ratings for the Digestive System. Ratings range from 0% for mild cases to 80% for severe conditions where only liquids can be passed and general health is markedly impaired.
The key to securing a rating is establishing service connection—proving the condition is directly, secondarily, or aggravated by military service. This requires comprehensive medical evidence, including diagnostic tests and a medical opinion linking the condition to service, to demonstrate the functional impact on a veteran’s daily life and ability to work.
Why This Update
The VA is constantly updating its policies and rating methods. We want to provide you with the most up-to-date content we can!
Tamila’s Take:
Swallowing may seem like a minor issue until it isn’t. When dysphagia interferes with eating, drinking, or breathing, it’s more than discomfort; it’s a serious health risk. Veterans should never ignore these symptoms or settle for a low rating if their daily life is affected.
Types of Dysphagia and Diagnostic Methods
Dysphagia presents in two primary forms, each with distinct characteristics and causes.
Oropharyngeal dysphagia affects the upper throat and mouth, making it challenging to start the swallowing process. This type is often linked to conditions affecting nerves or muscles that impact the coordination needed to move food from the mouth to the esophagus.
Esophageal dysphagia involves the esophagus itself, where food may feel stuck after swallowing begins. This form typically results from physical obstructions such as strictures, scarring from chronic GERD, or structural differences.
Common experiences across both types include frequent coughing or choking during meals, the sensation of food being stuck in the throat or chest, unintended weight loss, and persistent heartburn.
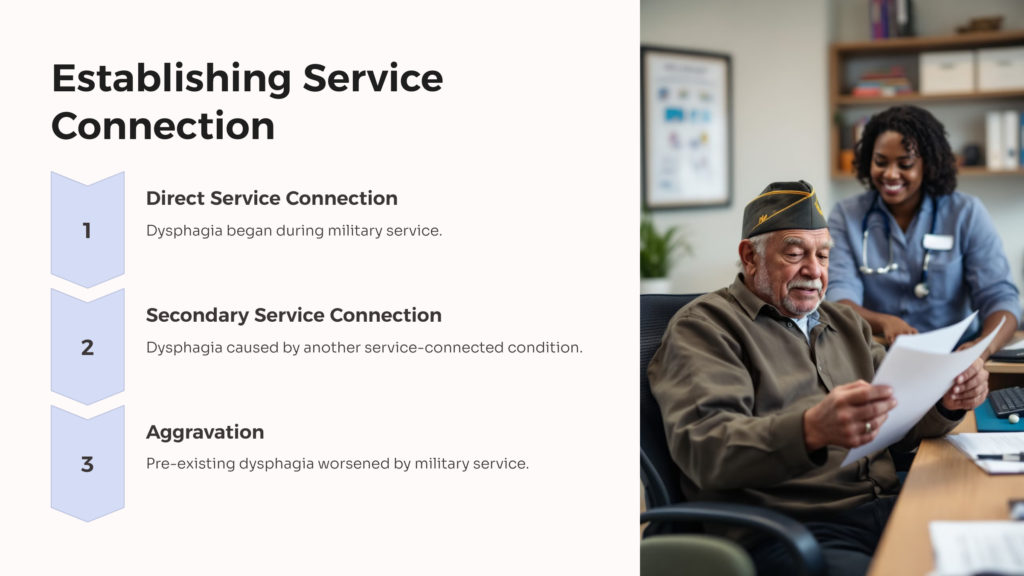
Proving Service Connection for Dysphagia
To receive VA disability benefits for dysphagia, you must show:
- A current medical diagnosis of dysphagia.
- An in-service event, illness, or injury that could have caused or aggravated the condition.
- A medical nexus linking your current condition to your service or to a service-connected condition.
Service-connected causes can include:
- Neck or spinal cord injuries
- TBI or stroke
- Radiation or surgery involving the throat
- Neurological disorders such as Parkinson’s or MS
Dysphagia is often filed as a secondary claim to already rated conditions. For instance, if you have a service-connected stroke or GERD, dysphagia could be added with supporting medical documentation.
Medical Evidence Needed to Win a Dysphagia VA Claim
Winning a claim means submitting the right evidence. You will need medical records confirming dysphagia diagnosis and severity. Swallow studies, such as Modified Barium Swallow or VFSS, showing aspiration risk or functional loss will also be required.
Nexus letters from doctors connecting dysphagia to your military service or another rated condition will further strengthen your claim. Lay statements describing how dysphagia affects your eating, breathing, or daily routine can also help.
Additionally, any documentation that shows the use of special diets, feeding tubes, weight loss, or malnutrition will solidify your case.
How the VA Rates Dysphagia (Diagnostic Codes and Criteria)
The VA typically rates dysphagia under Diagnostic Code 7203: Esophagus, stricture of. Ratings are assigned based on the level of functional impairment:
- 30%: Moderate stricture with occasional swallowing difficulty.
- 50%: Severe stricture requiring soft foods or a liquid-only diet.
- 80%: Marked stricture where only liquids can be swallowed, often accompanied by malnutrition or the need for feeding assistance.
In some cases, Diagnostic Code 7200, which is used for severe digestive tract complications, or 7346, typically used for hiatal hernia with reflux-related dysphagia, may be used if symptoms overlap.
VA Disability Percentages for Dysphagia and Related Conditions
A standalone dysphagia rating usually falls between 30% and 80%, depending on the symptoms’ frequency and severity. Veterans with co-occurring conditions like GERD, traumatic brain injury (TBI), ALS, or head and neck cancer may receive a secondary or combined rating.
Claims that involve a feeding tube or result in significant weight loss can justify higher ratings or even Total Disability Individual Unemployability (TDIU) if they impact daily function.
Document any secondary conditions that result from dysphagia, such as malnutrition, significant weight loss, aspiration pneumonia, or anxiety related to eating. These conditions may warrant separate ratings or support a higher rating for dysphagia itself.
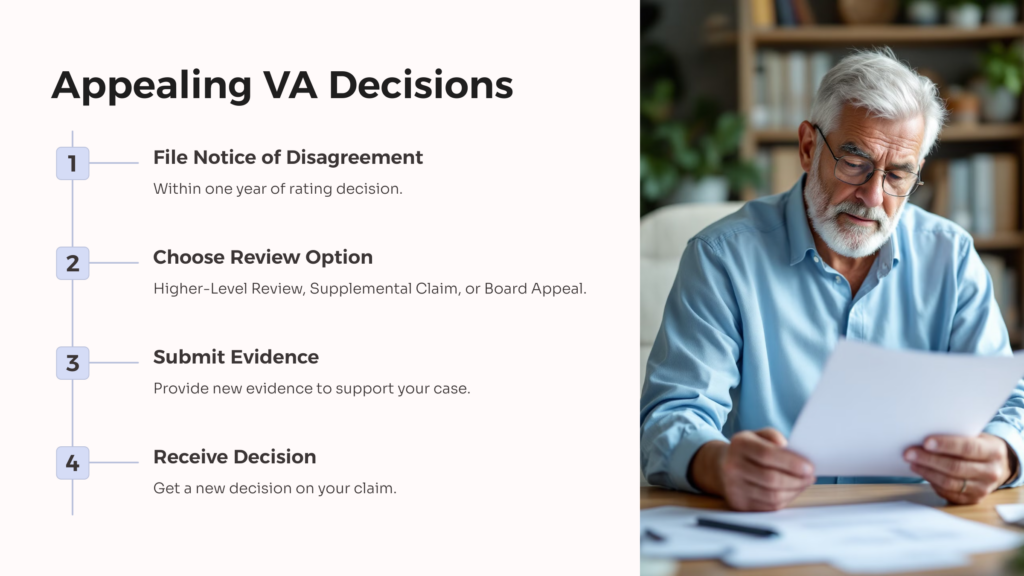
Appealing a VA Rating Decision
If you receive an unfavorable rating decision, you have the right to appeal. Understanding the appeals process and common obstacles may improve your chances of a successful outcome. You’re not alone in finding this process challenging.
You can appeal VA rating decisions by filing a Notice of Disagreement within one year of the decision letter date. The VA offers three appeal options. A Higher-Level Review involves a senior reviewer examining the same evidence without accepting new materials.
A Supplemental Claim allows submission of new and relevant evidence that was not previously considered. A Board Appeal brings the case before the Board of Veterans’ Appeals, with options for direct review, evidence submission, or a hearing. Common challenges in dysphagia claims include insufficient medical evidence that doesn’t adequately document severity and functional impact.
Clearly articulate functional limitations using specific examples rather than general descriptions. Instead of stating “I have trouble swallowing,” explain “I can only consume pureed foods and liquids, meals take 45 minutes or longer, and I’ve lost 30 pounds in six months.”
Working with a Veterans Service Organization (VSO) or VA-accredited attorney may improve appeal outcomes. These professionals understand VA procedures, know what evidence may strengthen claims, and can help you navigate the appeals system. They can also assist in obtaining independent medical examinations and nexus opinions that clarify the connection between dysphagia and military service.
What Receiving a VA Rating for Dysphagia Looks Like
Here’s a hypothetical example to consider when it comes to the VA rating for this condition. Sarah, a Navy veteran, developed severe reflux after her service. Over time, her GERD led to esophageal scarring, and she began having trouble swallowing even soft foods.
Her physician conducted a swallow study and confirmed moderate dysphagia. She submitted a secondary claim linked to her GERD and was awarded a 50% VA disability rating, with additional consideration for TDIU due to her inability to maintain employment.
FAQs About the VA Rating for Dysphagia
If you are dealing with dysphagia, it can be incredibly difficult to pinpoint a way forward with the VA. Here are some of the most frequently asked questions about this condition.
What is the VA diagnostic code for dysphagia?
Most dysphagia claims fall under Diagnostic Code 7203: Esophageal stricture.
Can dysphagia be a secondary VA condition?
Yes. In many cases, dysphagia is often secondary to GERD, head/neck injuries, stroke, or neurological disorders.
What’s the highest rating for dysphagia?
As noted above, the maximum rating for this condition is 80%. This is typically reserved for cases requiring a feeding tube or severe restriction of diet.
Do I need a swallow study to prove my claim?
A swallow study is not required. However, it will contribute additional evidence of your condition and can improve your chances of a more favorable rating.
Is dysphagia considered a presumptive condition?
Not typically. You must prove service connection unless it arises secondary to a presumptive condition like ALS.
Can I get TDIU for dysphagia?
Yes, if your symptoms prevent you from maintaining substantially gainful employment, you may qualify for TDIU.
What happens if I’m denied benefits for dysphagia?
You can appeal the decision, submit new evidence, or file a supplemental claim with updated medical documentation.
Don’t Let Dysphagia Go Underrated
It’s important not to allow your condition go underrated. Dysphagia can be life-altering, having an impact on your ability to eat, speak, and even breathe safely. For many veterans, it can be traced back to service-connected injuries or other conditions. But to receive the benefits you deserve, you will need to have a strong claim backed by medical evidence and a clear service connection.
If you’re unsure how to document your symptoms or connect dysphagia to your service, AllVeteran.com can help. Our free medical evidence screening is designed to uncover gaps in your claim and strengthen your case. Don’t let your voice or your benefits be silenced. Get the support you’ve earned.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.


















