Life after military service can present unique challenges, both physical and psychological. Fortunately, the Department of Veterans Affairs (VA) offers support through disability claims, providing vital assistance to those who have served their country. These claims, representing different kinds of injuries and conditions, are essential in ensuring veterans receive the care and compensation they rightfully deserve.
The importance of VA disability claims cannot be overstated. They serve as a lifeline for veterans, offering financial support, access to healthcare, and acknowledgment of their sacrifices in service to the nation.
Each fiscal year, the United States Department of Veterans Affairs publishes a benefits report that lists the annual most common disabilities among veterans.
According to the VA’s annual benefits reports, here are the top 20 most common VA disability claims.
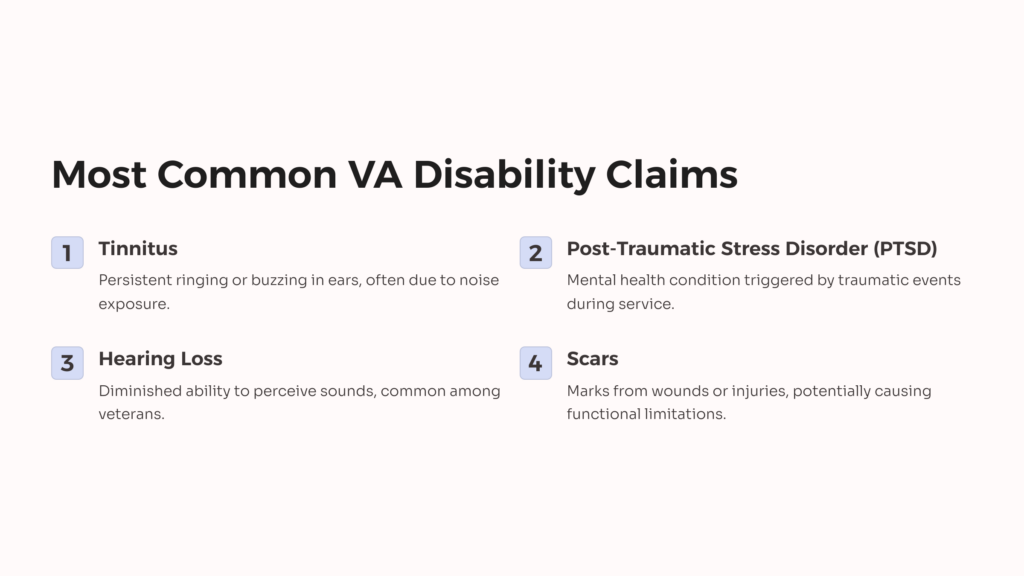
#1. Tinnitus
Tinnitus, a persistent ringing, buzzing, or hissing sound in the ears, affects several veterans globally. It’s often a symptom of underlying health conditions such as hearing loss, ear injuries, or neurological disorders. Exposure to high levels of noise from combat situations, machinery, and aircraft can significantly increase the risk of developing tinnitus among service members.
Veterans frequently encounter intense noise levels during their deployments or training exercises, leading to long-term repercussions on their hearing health.
Veterans do not need to be specifically diagnosed with tinnitus before they’re granted service connection. They can submit a subjective report of their symptomatology, enough to meet the rating criteria.
Tinnitus is rated under 38 CFR § 4.87, Diagnostic Code 6260. The highest scheduler rating for tinnitus, taking both ears into account, is 10%.
Veterans rarely receive hugger ratings on an extra-schedular basis.
#2. Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a traumatic event. Symptoms may include intrusive memories, flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event. Individuals with PTSD may also experience hypervigilance, avoidance of reminders of the trauma, and mood swings.
PTSD is common among military service retirees due to the high-stress nature of combat situations and the exposure to traumatic events. Service members often face life-threatening situations, witness violence, and endure prolonged periods of stress during deployments. These experiences can lead to the development of PTSD, impacting the mental health and well-being of military personnel.
The unique challenges of military service, including exposure to combat, loss of comrades, and multiple deployments, increase the risk of PTSD among veterans.
PTSD is rated under the schedule of Mental Disorder rating, 38 CFR § 4.130, Diagnostic Code 9411, at 0, 30, 50, 70, or 100 percent.
Rating is determined by the severity of social and occupational impairments, including the duration, frequency, and symptom severity.
#3. Hearing loss
Hearing loss refers to a diminished ability to perceive sounds, ranging from mild to profound impairment. It can be caused by exposure to loud noises, aging, genetic predisposition, infections, and certain medical conditions or treatments.
Exposure to high noise levels is a leading cause of hearing loss among service members. Combat environments are inherently noisy, with gunfire, explosions, machinery, and aircraft generating intense sound. Prolonged exposure to these loud noises without adequate hearing protection can damage the delicate structures of the inner ear, leading to permanent hearing loss.
According to the Centers for Disease Control, veterans experience 30% higher rates of hearing impairment compared to the general population. The nature of military operations exposes service members to hazardous noise levels, increasing their risk of developing hearing loss over time. As a result, hearing loss ranks among the most common service-connected disabilities claimed by veterans.
Hearing loss ratings are usually based on two auditory tests required by the VA to confirm hearing loss:
- Speech discrimination (Maryland CNC Test)
- Pure tone threshold (Puretone Audiometric Test)
Ratings range from 0-100%, with 0 to 100% common among veterans.
#4. Scars
Scars are marks left on the skin’s surface after a wound or injury has healed. They are a natural part of the body’s healing process and can vary in size, shape, and appearance depending on the type and severity of the injury. Scars can result from various causes, including accidents, surgeries, burns, lacerations, and medical conditions such as acne or infections.
While scars themselves are not inherently disabling, they can lead to functional limitations and psychological distress depending on their location, size, and severity. For example, scars near joints or flexible body areas may restrict movement and cause discomfort or pain.
Rated under 38 CFR § 4.87, Diagnostic Code 7800-7805, scars may be considered disabling if they result from service-related injuries or conditions. Veterans who have sustained scars during their military service may be eligible for VA disability compensation if the scars cause functional impairment, such as limited range of motion, chronic pain, or psychological distress.
The VA evaluates scars based on their impact on veterans’ ability to perform daily activities and their overall quality of life, providing compensation and healthcare benefits to eligible veterans.
Scars are rated anywhere from 0 to 80 percent by the diagnostic code.
#5. Joint injuries/joint pain
Joint injuries and pain can significantly impact mobility and quality of life. These conditions include various issues affecting the joints, including strains, sprains, arthritis, and more severe injuries such as fractures or dislocations. Common causes of joint injuries and pain include trauma from accidents, overuse or repetitive motion, degenerative conditions like osteoarthritis, and inflammatory diseases such as rheumatoid arthritis.
Joint injuries and pain are prevalent in military service due to the physical demands placed on service members during training and combat. Soldiers often engage in strenuous activities, carry heavy loads, and may endure repetitive movements, all of which can increase the risk of joint injuries and exacerbate existing conditions. Additionally, exposure to harsh environmental conditions and carrying heavy gear over extended periods can contribute to wear and tear on the joints, leading to chronic pain and disability.
The rigorous nature of military training and operations can damage the musculoskeletal system, leading to acute injuries or the development of chronic joint conditions.
#6. Lumbar and cervical strains
Lumbar and cervical strains refer to injuries affecting the muscles and ligaments in the lower back (lumbar region) and neck (cervical region). These strains often result from sudden movements, overexertion, or improper lifting techniques, stretching or tearing the soft tissues surrounding the spine. Common symptoms include pain, stiffness, limited range of motion, and muscle spasms in the affected area.
Lumbar and cervical strains are prevalent due to soldiers frequently engaging in tasks that require heavy lifting, carrying equipment, and maintaining awkward positions for extended periods.
The rigorous nature of military training and operations and the need to perform physically demanding tasks in challenging environments can predispose service members to lumbar and cervical strains. Whether caused by lifting heavy gear, jumping from vehicles, or navigating rough terrain, these strains can result in acute pain and functional limitations that impact a service member’s ability to carry out duties effectively.
Repetitive stress and cumulative trauma over time can contribute to the development of chronic lumbar and cervical strain conditions among military personnel. These injuries not only affect readiness and performance but also have long-term implications for veterans transitioning to civilian life. VA ratings for conditions such as lumbar and cervical strains are backed under 38 CFR § 4.71a, Schedule of Ratings, Musculoskeletal System, and eligibility is largely based on a veteran’s range of motion. Ratings range from 0 to 100%.
#7. Paralysis of the Sciatic Nerve
Paralysis of the sciatic nerve is the loss of motor function and sensation in the lower extremities due to damage or compression of the largest nerve in the body, the sciatic nerve. This condition can result from various causes, including trauma, spinal cord injuries, herniated discs, tumors, or prolonged pressure on the nerve.
In military service, paralysis of the sciatic nerve may occur as a result of combat injuries, falls, vehicle accidents, or other traumatic events. Service members operating in combat zones or engaging in physically demanding activities are at risk of sustaining injuries that can damage the sciatic nerve and lead to paralysis. Prolonged periods of sitting, standing, or carrying heavy loads during deployments can contribute to nerve compression and subsequent paralysis. The demanding nature of military service increases the likelihood of traumatic injuries to the spine and nerves, highlighting the connection between military service and paralysis of the sciatic nerve.
#8. Limitation of Range of Motion of the Ankle
Limitation of range of motion (ROM) of the ankle refers to reduced flexibility and movement in the ankle joint, making it difficult to perform activities such as walking, running, or climbing stairs. Causes of limited ankle ROM may include sprains, fractures, arthritis, tendon injuries, or previous surgeries.
Ankle ROM can be limited due to injuries sustained during training exercises, combat operations, or physical conditioning activities. Soldiers may experience ankle sprains from uneven terrain, fractures from falls or impacts, or tendon injuries from repetitive stress or overuse. The demanding and often hazardous nature of military environments increases the risk of ankle injuries among service members, impacting their ability to fulfill their duties effectively.
The need for rapid movement, carrying heavy loads, and navigating challenging terrain during deployments can exacerbate existing ankle conditions or lead to new injuries, resulting in decreased ankle ROM. Limitation of motion in the ankle is rated under 38 CFR § 4.71, with Schedule of Ratings, Musculoskeletal System, and Diagnostic Code 5271, at 10 or 20%.
#9. Migraines
Migraines are neurological disorders characterized by recurrent, severe headaches often accompanied by symptoms such as nausea, vomiting, sensitivity to light and sound, and visual disturbances. They can significantly impair daily functioning and quality of life for those affected.
Migraines may be linked to various factors, including stress, sleep disturbances, exposure to environmental triggers, and head injuries sustained during training or combat. The high-stress environment of military life, combined with irregular sleep patterns and exposure to loud noises or bright lights, can exacerbate migraine symptoms among service members. Additionally, deployment-related stressors, such as combat experiences, separation from loved ones, and unpredictable schedules, may increase the risk of migraine attacks.
The physical and psychological toll of military service, coupled with the potential for head injuries and exposure to migraine triggers, underscores the connection between migraines and military service. Recognizing and addressing the impact of migraines on service members’ health and readiness is essential for providing appropriate care and support to those affected.
#10. Limitation of Arm Motion
Limitation of arm motion refers to a restricted or decreased range of motion in the shoulder, elbow, or wrist joints, making it difficult to perform everyday tasks such as lifting, reaching, or carrying objects. This condition can result from various causes, including injuries, musculoskeletal disorders, nerve damage, or previous surgeries.
Limitation of arm motion is commonly linked to injuries sustained during training exercises, combat operations, or physical conditioning activities. Veterans may experience shoulder dislocations, fractures, rotator cuff tears, or nerve injuries from falls, impacts, overuse, or direct trauma.
Repetitive movements, heavy gear, and prolonged periods of carrying equipment can contribute to wear and tear on the shoulder and arm joints, leading to a decreased range of motion.
Traumatic events such as explosions, blasts, or vehicle accidents can result in traumatic injuries to the upper extremities, including fractures, nerve damage, or soft tissue injuries, which may lead to long-term limitations in arm motion. The physical demands and hazards associated with military service increase the risk of shoulder and arm injuries among service members. VA backs up its rating under 38 CFR § 4.71a, Diagnostic Code 5201, at 20, 30, or 40 percent.
VA considers whether the condition affects the veteran’s dominant or non-dominant arm, including the severity.
#11. Impairment of the knee
Impairment of the knee refers to any condition or injury that hampers the normal function of the knee joint. Symptoms may include pain, swelling, stiffness, instability, and reduced range of motion. This impairment can stem from various causes, such as ligament tears (like ACL or MCL), meniscus tears, cartilage damage, arthritis, or fractures.
Knee impairments are frequently linked to the physical demands of training and combat activities. Soldiers often engage in rigorous training exercises, carry heavy loads, navigate challenging terrain, and frequently perform repetitive motions that can strain the knee joint. Additionally, combat situations increase the risk of traumatic injuries due to explosions, falls, or direct impact.
The nature of military duties can exacerbate pre-existing knee conditions or lead to new injuries, resulting in impairment. Such impairments can significantly impact a service member’s ability to perform their duties effectively and may require medical treatment, physical therapy, or surgical intervention. Consequently, knee impairments are a common cause of disability among military personnel, affecting their quality of life and potentially leading to medical discharge or limitations in duty assignments.VA backs up its rating under 38 CFR § 4.71a, Diagnostic Code 5260, at usually 40 percent.
#12.Traumatic Brain Injury
Traumatic Brain Injury (TBI) refers to damage to the brain caused by a sudden, external force, such as a blow, jolt, or penetrating injury to the head. Symptoms of TBI can vary widely depending on the severity and location of the injury. Still, they may include headaches, dizziness, confusion, memory problems, difficulty concentrating, mood changes, and loss of consciousness.
TBI is commonly linked to combat-related incidents such as blasts from improvised explosive devices (IEDs), direct blows to the head, falls, or vehicle accidents. Explosions are a significant cause of TBI in military personnel due to the concussive force generated, even without direct impact to the head. The high-pressure shockwaves from explosions can cause brain injuries ranging from mild concussions to severe trauma, often referred to as blast-related TBI.
Training exercises, sports activities, and other hazards encountered during military service can also result in TBI. The prevalence of TBI among service members has drawn increased attention in recent years due to its potential long-term consequences, including cognitive impairment, emotional disturbances, and increased risk of neurodegenerative disorders like chronic traumatic encephalopathy (CTE). As a result, TBI has become a significant focus of research, treatment, and support efforts within the military community.
VA’s rating of TBI under 38 CFR § 4.124a is based on the current residual symptoms a veteran experiences due to the trauma.
TBI residual rating criteria are divided into 10 categories to determine the condition based on impairment and severity level of each area. Ratings range from 0 to 100%.
#13. Diabetes Mellitus (Type 2)
Diabetes Mellitus (Type 2) is a chronic condition characterized by high blood sugar levels due to insufficient insulin production or the body’s ineffective use of insulin. Symptoms may include increased thirst, frequent urination, fatigue, blurred vision, and slow wound healing. In military service, Type 2 diabetes is often associated with lifestyle factors among soldiers, such as poor diet, lack of exercise, and obesity, as well as genetic predisposition.
Additionally, exposure to certain environmental factors during deployment, such as stress, disrupted sleep patterns, and dietary changes, can contribute to the development of Type 2 diabetes among service members.
VA backs up its rating under 38 CFR § 4.119a, Diagnostic Code 7913, at 10,20, 40, 60, and 100 percent.
#14. Sleep Apnea
Sleep Apnea is a sleep disorder characterized by pauses in breathing or shallow breathing during sleep. Symptoms may include loud snoring, gasping for air during sleep, daytime sleepiness, irritability, and difficulty concentrating. In military service, sleep apnea is commonly linked to factors such as obesity, older age, male gender, and specific anatomical characteristics. Deployment-related stress, irregular sleep schedules, and exposure to environmental factors like high altitudes or poor air quality can also increase the risk of sleep apnea among service members.
The VA will ask to conduct a sleep study to determine a sleep apnea diagnosis for compensation.
#15. Bronchial Asthma
Bronchial Asthma is a chronic respiratory condition characterized by airway inflammation, leading to wheezing, coughing, chest tightness, and shortness of breath. In military service, bronchial asthma can be triggered or exacerbated by exposure to various environmental factors such as dust, smoke, pollution, allergens, and chemical agents.
Deployment to areas with high levels of airborne contaminants or allergens and strenuous physical activity can increase the risk of developing or worsening asthma among service members.
#16. Residuals of Traumatic Amputation
Residuals of Traumatic Amputation refer to the long-term effects and complications resulting from the loss of a limb due to traumatic injury. Common symptoms include phantom limb pain, neuromas, musculoskeletal issues, and psychological challenges such as depression and anxiety.
Traumatic amputations often occur as a result of combat-related injuries, explosions, or accidents. The physical and emotional impact of limb loss can significantly affect a service member’s quality of life, requiring ongoing medical care, rehabilitation, and support services.
#17. Ischemic Heart Disease
Ischemic Heart Disease is characterized by reduced blood flow to the heart muscle, typically due to coronary artery disease (atherosclerosis). Symptoms may include chest pain or discomfort (angina), shortness of breath, fatigue, and heart palpitations. Ischemic heart disease can be linked to various risk factors such as smoking, high blood pressure, high cholesterol, obesity, physical inactivity, and stress.
Deployment-related factors such as exposure to environmental hazards, dietary changes, and psychological stressors can also contribute to the development or exacerbation of ischemic heart disease among service members.
#18. Arteriosclerotic Heart Disease (ASHD)
Arteriosclerotic Heart Disease (ASHD), also known as coronary artery disease, is characterized by plaque buildup in the arteries supplying blood to the heart muscle. Symptoms and risk factors are similar to those of ischemic heart disease, including chest pain, shortness of breath, and cardiovascular risk factors such as smoking, high blood pressure, high cholesterol, obesity, and physical inactivity.
Military service can contribute to the development or worsening of ASHD through deployment-related stressors, exposure to environmental toxins, and lifestyle factors.
#19.Hypertensive Vascular Disease (HVD)
Hypertensive Vascular Disease (HVD) refers to a group of conditions affecting the blood vessels, including hypertension (high blood pressure) and its associated complications such as stroke, heart attack, and peripheral artery disease.
In military service, HVD can be linked to various factors such as stress, physical inactivity, poor diet, smoking, alcohol consumption, and genetic predisposition. Deployment-related stressors and exposure to environmental factors can also contribute to the development or exacerbation of HVD among service members. VA backs up its rating under 38 CFR § 4.130a, Diagnostic Code 7913, at 10,20,40,60 and 100 percent.
#20. Depressive Disorder
Depressive Disorder comes with mood disorders characterized by persistent feelings of sadness, hopelessness, and loss of interest or pleasure in activities. Symptoms may also include changes in appetite or weight, sleep disturbances, fatigue, difficulty concentrating, and thoughts of suicide or self-harm. They’re commonly associated with deployment-related stressors such as combat exposure, separation from family, traumatic experiences, and adjustment difficulties. Pre-existing factors such as genetics, childhood experiences, and past trauma can increase the risk of depression among service members.
Tips to make a successful VA claim

Making a successful VA disability claim involves thorough preparation, attention to detail, and understanding of the filing process. These tips can help you go through the VA disability claims process effectively:
Understanding Eligibility Criteria
Before initiating a claim, ensure you meet the eligibility criteria for VA disability benefits. Generally, you must be a veteran with a service-connected disability or a condition aggravated by military service.
Gather Important Documents
Collect relevant documents to support your claim, including:
- Military service records (DD-214)
- Medical records documenting your injury or condition
- Supporting statements from medical professionals, fellow service members, or family members
- Any other relevant documentation, such as accident reports or incident records
Seek Medical Evaluation
Obtain a thorough medical evaluation of your condition from a qualified healthcare provider. Make sure your medical records accurately reflect the severity and impact of your disability on your daily life and functioning.
Understanding VA Disability Ratings
Familiarize yourself with the VA’s Schedule for Rating Disabilities (VASRD) to understand how disabilities are rated and compensated based on their severity and impact on your ability to work and perform daily activities.
File Your Claim
Choose the most suitable method to file your claim:
- Online through the VA’s eBenefits portal or VA.gov
- By mail using VA Form 21-526EZ (Application for Disability Compensation and Related Compensation Benefits)
Provide Detailed Information
Complete your claim form accurately and provide detailed information about your medical history, service-related injuries or conditions, and how they affect your daily life and ability to work.
Follow Up and Stay Informed
You can track your claim status through the VA’s online portal or by contacting the VA directly. Be prepared to respond promptly to requests for additional information or medical examinations.
Consider Seeking Assistance
If you encounter challenges or need assistance with your claim, consider seeking help from veterans service organizations (VSOs), accredited claims agents, or legal professionals specializing in VA disability claims.
These steps and tips can increase your chances of making a successful VA disability claim and receiving the benefits you deserve for your service-connected disabilities.
Wrapping Up
Understanding the most common VA disability claims is crucial for veterans as it enables them to recognize and address the health issues they may be facing as a result of their military service. By identifying these common conditions, veterans can take proactive steps to seek the support and benefits they rightfully deserve from the Department of Veterans Affairs (VA).
Check out Allveteran.com for a valuable resource on how to undergo the claims process and access the benefits you’re entitled to. Whether you need assistance with filing claims, accessing healthcare services, or connecting with other veterans for support, Allveteran.com offers comprehensive assistance tailored to veterans’ needs.
You must take advantage of the resources available and start claiming your benefits. By doing so, you improve your well-being and honor your service and sacrifice to the nation. Visiting Allveteran.com empowers you to take control of your health and receive the support you deserve as you transition to civilian life.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.


















