Chest pain is often a sign of serious medical issues. Especially as we age, paying attention to chest pain can quite literally be the difference between life and death. But not every pain in the chest is caused by something urgent, life-threatening, or catastrophic. Still, it can prove disruptive and hamper your ability to handle normal responsibilities, like work.
So, can you still get VA disability benefits if the aching you feel in your torso is arguably “non-mission critical?”
Potentially, yes. And a VA disability claim is definitely worth a try. Just because one squadmate has it worse doesn’t mean your pain is any less valid. You are equally deserving of VA disability benefits appropriate to your level of need.
So, let’s brief you on the details and need-to-know intel.
Understanding Costochondritis
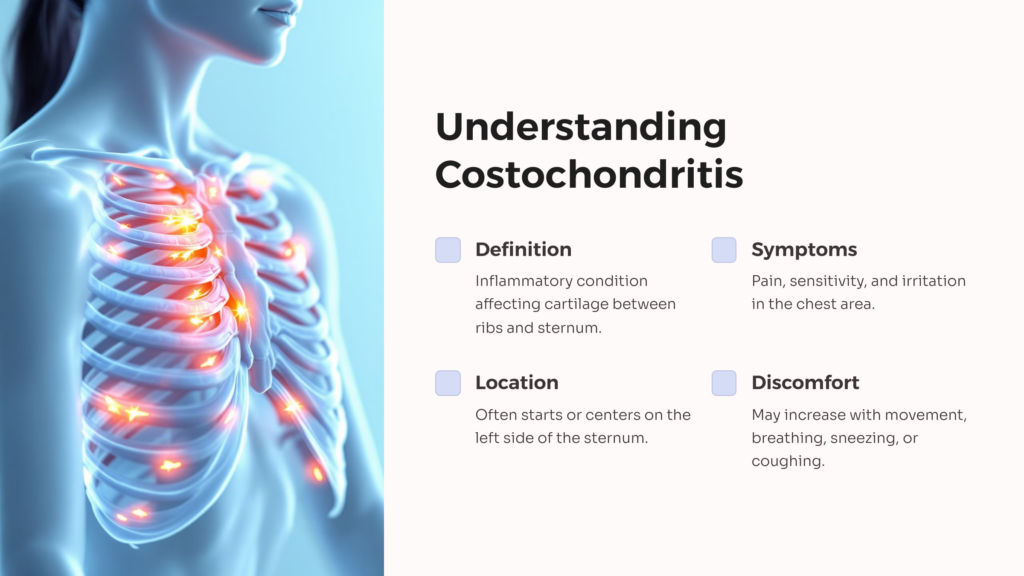
As we alluded to above, there are a few different ways you can end up with chest pain. For this article, we’ll be focusing on one in particular: costochondritis. Another medical condition with a complicated name and minimal visibility to the general public, costochondritis is an inflammatory condition that affects the cartilage between the ribs and the sternum (breastbone).
Like all inflammatory conditions (and inflammation in general), it comes standard-issue with symptoms like pain, sensitivity, and irritation. The type of pain can vary—it might be an ache, a pressure, or a sharp sensation. But it will likely start or center on the left side of your sternum (though it may radiate out from there).
Similar to what you might feel with bruised or broken ribs, you might experience added discomfort when moving or doing anything strenuous, like, say, breathing (or sneezing, or coughing, or…).
Potential Causes and Risk Factors
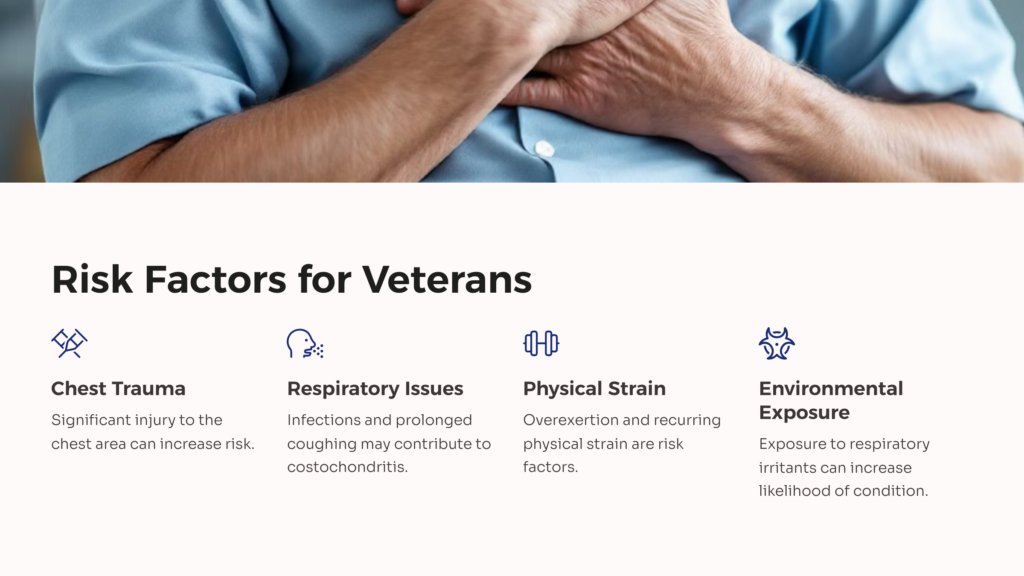
Inflammatory conditions are notoriously difficult to find causes for. Inflammation is a normal biological response to infections, injuries, and a variety of other concerns our bodies deal with on basically a daily basis. It’s one of the first things the body will do in an effort to heal and repair itself. In other words, in the absence of a clear trigger, inflammation could be the result of just about anything. Bottom line: the root cause of costochondritis has yet to be determined.
We are aware of some pretty significant risk factors, things that dramatically increase the likelihood that you’ll end up with the condition. And, as you might expect, much of the list consists of things veterans are well acquainted with:
- Significant trauma or injury to the chest
- Overexertion and recurring physical strain
- Respiratory tract infections
- Infection of a chest wound
- Severe and prolonged coughing
- Excessive exposure to extreme respiratory irritants
It’s also more likely to occur in people over the age of 40 and is more commonly found in women than in men.
“Is This a Heart Attack?”
Costochondritis shares a number of key symptoms with other conditions. For example, severe pain focused on the left side of the ribcage is also a potential sign of a heart attack. Unlike a heart attack, though, costochondritis doesn’t carry the same life-threatening urgency.
Another example is Tietze syndrome. This rare condition is similar in many ways to costochondritis but also involves swelling of the cartilage tissue. While it’s possible to experience both simultaneously, leading to both inflammation and swelling, Tietze is rare, and it’s much more likely that you’re only dealing with just inflammation.
“Give It to Me Straight, Doc; How Bad Is It?”
Diagnosing costochondritis usually involves blood tests, potentially a round or two of X-rays, and possibly an electrocardiogram (ECG) test. Once you’re diagnosed, treatment is focused on reducing inflammation and pain, giving the affected tissue time to heal and recover.
The condition is almost always temporary, and is almost always manageable with standard over-the-counter anti-inflammatory medications. In a few cases, you may need some additional help reducing the inflammation in the form of steroids (not unlike how patients with asthma, allergies, or recent organ transplants are treated).
Ultimately, the prognosis is generally positive. Most patients recover over time with treatment. And while there are some minimal risks of complications, most see their symptoms clear up in weeks or months.
Despite this, the severe pain and discomfort can interfere with a vet’s ability to perform physical activity and manual labor, leading to difficulty maintaining employment.
Vets and Costochondritis
Establishing Service Connection
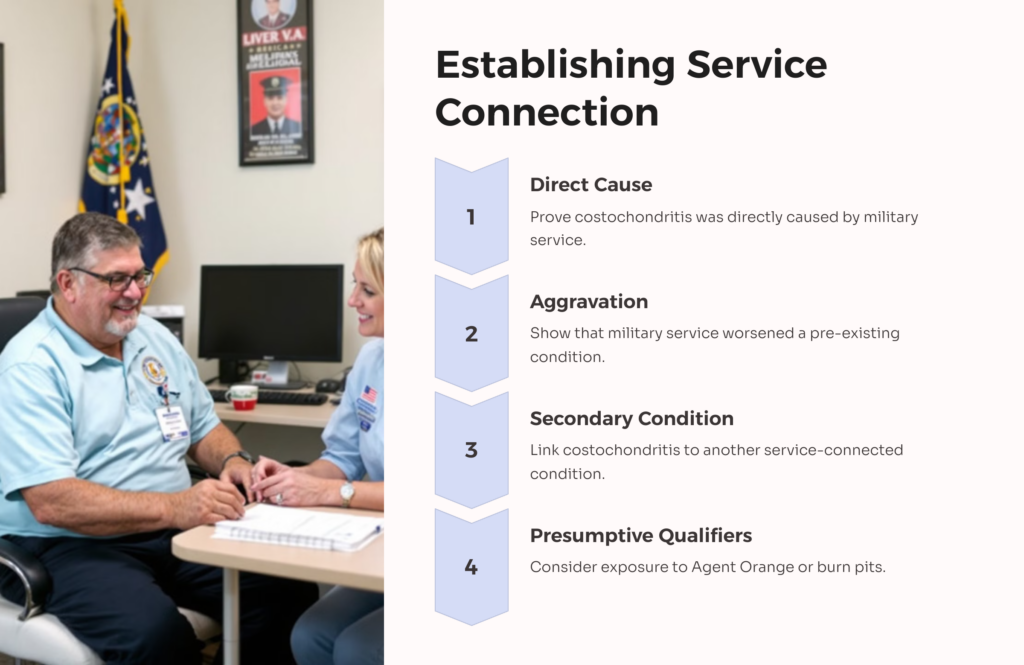
Veterans are exposed to a variety of situations that might lead to this condition. Military service tends to involve a lot of physical activity and a heightened risk of injury, to put it mildly. Beyond this, though, certain big risk factors are worth noting, especially due to their status as “presumptive” automatic qualifiers. These include exposure to Agent Orange and burn pits.
Service connection can be established via direct cause of the costochondritis condition, by proving aggravation of the condition, or by pinpointing it as a secondary condition.
Costochondritis VA Rating
As far as getting a VA disability rating for costochondritis, it’s important to know that there’s not currently a separate diagnostic code for this one. That said, it can be rated as an analogous condition—in this case, a musculoskeletal disability affecting that particular region of the body.
Once you submit your VA disability claim, they will look at your medical record and your symptoms before assigning your VA disability rating. The higher the rating, the more VA benefits you can recieve.

For veterans who deal with difficulty from “moderately severe” to “severe,” they can qualify for a rating of 20%. If the impact on functionality is only “moderate,” they may qualify for 10%. Below that, they’ll receive a rating of 0%.
The rating you receive for costochondritis can also be used in the VA disability calculator used to determine TDIU (total disability based on individual unemployability).
Setting aside everything we said about this condition not being life-threatening, “it hurts when I breathe” is still a rough hand to be dealt. Urgent or not, temporary or not, you deserve the help you need, especially when that need is a direct result of your time in the service.
If you’re interested in learning more, and maybe getting a free medical evidence screening, visit AllVeteran.com and take our quiz.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.