A hiatal hernia is a condition where part of the stomach pushes up through the diaphragm, the muscle that separates the chest from the abdomen. This can cause various symptoms, including heartburn, chest pain, and difficulty swallowing. For veterans, hiatal hernias can be particularly troublesome, as they may be caused or worsened by military service.
Veterans with hiatal hernias often experience a significant impact on their daily lives. The condition can interfere with eating, sleeping, and physical activities. Some veterans may find that their hiatal hernia symptoms are triggered or exacerbated by stress, which is common among those who have served in the military.
The Department of Veterans Affairs (VA) recognizes hiatal hernia as a service-connected disability, meaning veterans may be eligible for benefits if their condition is related to their military service. Understanding how the VA rates hiatal hernias is crucial for veterans seeking compensation and support for their condition.
How the VA Rates Hiatal Hernia
The VA rates hiatal hernias under the digestive system category in the VA Schedule for Rating Disabilities. Specifically, hiatal hernias are evaluated under Diagnostic Code 7346. The rating system is designed to assess the severity of symptoms and their impact on a veteran’s daily life and ability to work.
When rating a hiatal hernia, VA examiners consider several factors:
1. The frequency and severity of symptoms
2. The impact on overall health
3. The presence of associated conditions, such as gastroesophageal reflux disease (GERD)
4. The effectiveness of treatment
The VA uses a percentage-based system to rate disabilities, with higher percentages indicating more severe conditions. For hiatal hernias, the ratings range from 10% to 60%, depending on the symptoms and their impact on the veteran’s life.
It’s important to note that the VA may consider secondary conditions related to hiatal hernias when determining the overall disability rating. This means that if a veteran develops additional health issues as a result of their hiatal hernia, these may also be factored into their disability compensation.
Understanding the Rating Percentages: 10%, 30%, and 60%
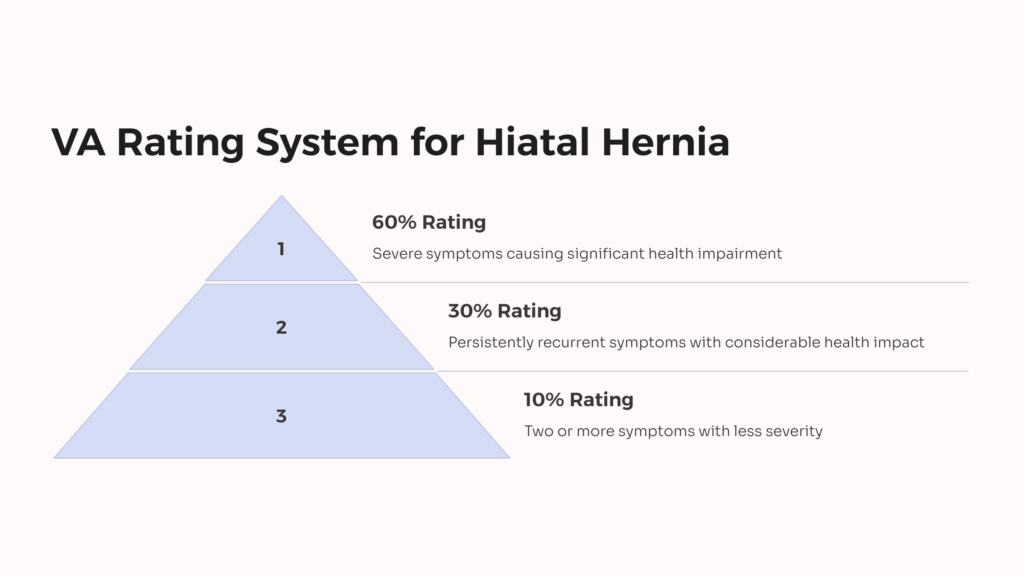
The VA assigns three main rating percentages for hiatal hernias: 10%, 30%, and 60%. Each rating corresponds to a specific set of symptoms and their severity. Let’s break down what each rating means:
10% Rating: A 10% rating is assigned when a veteran experiences two or more of the symptoms for the 30% rating, but with less severity. This might include occasional heartburn, regurgitation, or mild difficulty swallowing.
30% Rating: To qualify for a 30% rating, a veteran must have persistently recurrent epigastric distress with dysphagia (difficulty swallowing), pyrosis (heartburn), and regurgitation, accompanied by substernal or arm or shoulder pain. These symptoms should be productive of considerable impairment of health.\
60% Rating: The highest rating of 60% is reserved for the most severe cases. This rating is assigned when symptoms of pain, vomiting, material weight loss, and hematemesis or melena with moderate anemia are present. Alternatively, other symptom combinations that are productive of severe impairment of health can also qualify for a 60% rating.
It’s crucial for veterans to accurately report their symptoms and how they affect daily life when applying for VA disability benefits. The more detailed and well-documented the evidence, the better chance of receiving an appropriate rating.
Eligibility Criteria for VA Rating
To be eligible for a VA rating for hiatal hernia, veterans must meet certain criteria. The primary requirements are:
1. Current Diagnosis: The veteran must have a current diagnosis of hiatal hernia from a qualified medical professional.
2. Service Connection: The hiatal hernia must be connected to the veteran’s military service. This can be established in three ways:
3. Direct Service Connection: The condition developed during active military service.
4. Secondary Service Connection: The hiatal hernia was caused or aggravated by another service-connected condition.
5. Presumptive Service Connection: In some cases, the VA presumes certain conditions are related to specific types of military service.
6. Medical Evidence: There must be medical evidence linking the current hiatal hernia to the veteran’s military service or a service-connected condition.
7. Severity of Symptoms: The severity of the hiatal hernia symptoms must meet the VA’s rating criteria to qualify for compensation.
Veterans should gather all relevant medical records, service records, and any other documentation that supports their claim. This might include statements from fellow service members or family members who can attest to the onset or worsening of symptoms.
It’s also important to note that veterans can apply for benefits even if their hiatal hernia developed after leaving the military, as long as they can prove it’s connected to their service.
The VA Claims Process for Hiatal Hernia
Navigating the VA claims process for hiatal hernia can be complex, but understanding the steps can help veterans prepare a strong claim. Here’s an overview of the process:
1. Gather Evidence: Collect all medical records, service records, and any other documentation related to your hiatal hernia and its connection to your military service.
2. File a Claim: Submit VA Form 21-526EZ, Application for Disability Compensation and Related Compensation Benefits. This can be done online through the VA’s eBenefits portal, by mail, or in person at a VA office.
3. VA Review: The VA will review your claim and may request additional information or schedule a Compensation and Pension (C&P) exam.
4. C&P Exam: If required, attend the C&P exam. This is an opportunity for a VA-approved doctor to assess your condition and its severity.
5. Decision: The VA will make a decision on your claim, assigning a rating if your claim is approved.
6. Appeal: If you disagree with the decision, you have the right to appeal.
Throughout this process, it’s crucial to be thorough and timely in your responses to VA requests. Many veterans find it helpful to work with a Veterans Service Organization (VSO) or a VA-accredited attorney to navigate the claims process.
Remember, the goal is to provide a clear picture of how your hiatal hernia affects your daily life and how it’s connected to your military service. Be honest and detailed in describing your symptoms and their impact.
Common Symptoms that Affect Your Rating
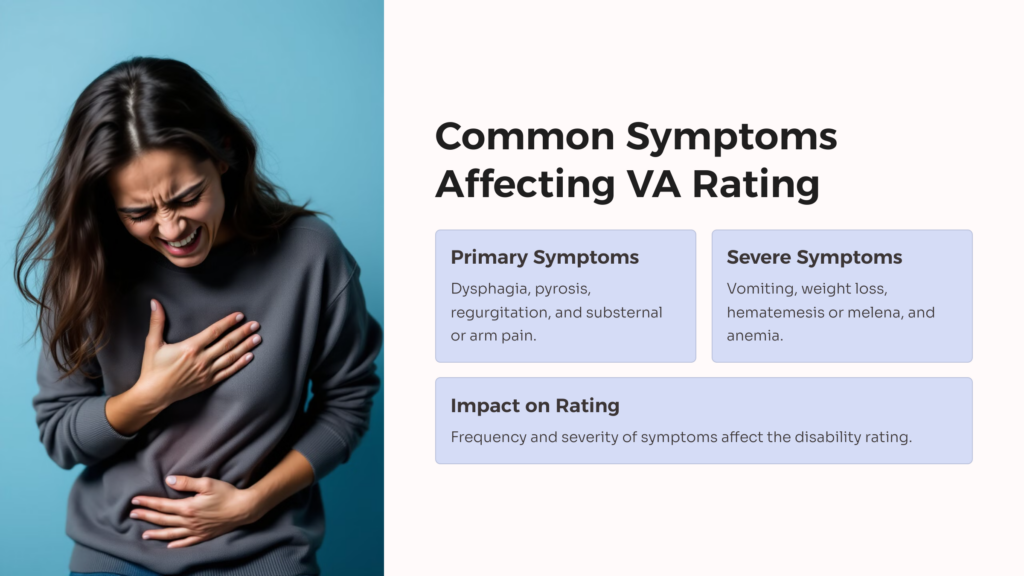
When evaluating a hiatal hernia for VA disability rating purposes, certain symptoms carry more weight than others. Understanding these key symptoms can help veterans better communicate their condition to VA examiners. Here are some of the most important symptoms that can affect your rating:
1. Dysphagia: Difficulty swallowing is a significant symptom. The severity and frequency of dysphagia can greatly impact your rating.
2. Pyrosis: Also known as heartburn, this burning sensation in the chest or throat is a common and often distressing symptom of hiatal hernia.
3. Regurgitation: The backflow of stomach contents into the mouth can be both uncomfortable and embarrassing, affecting quality of life.
4. Substernal, Arm, or Shoulder Pain: Pain that radiates to these areas can indicate a more severe condition and may lead to a higher rating.
5. Vomiting: Frequent vomiting, especially if it leads to weight loss or malnutrition, is considered a severe symptom.
6. Hematemesis or Melena: Vomiting blood or passing black, tarry stools are serious symptoms that can significantly increase your rating.
7. Weight Loss: Unintentional weight loss due to eating difficulties or persistent symptoms can indicate a more severe condition.
8. Anemia: If your hiatal hernia leads to anemia, it may be considered evidence of a more serious health impact.
It’s important to keep a detailed record of these symptoms, including their frequency, severity, and impact on daily activities. This information can be crucial in ensuring you receive an appropriate VA disability rating for your hiatal hernia.
How GERD is Related to Hiatal Hernia
Gastroesophageal reflux disease (GERD) and hiatal hernia are closely related conditions that often occur together. Understanding this relationship is important for veterans seeking VA benefits, as the presence of GERD can impact the overall disability rating for a hiatal hernia.
GERD is a chronic digestive disorder where stomach acid frequently flows back into the esophagus. This backwash (acid reflux) can irritate the lining of the esophagus, causing symptoms such as heartburn, difficulty swallowing, and chest pain. Many of these symptoms overlap with those of a hiatal hernia.
A hiatal hernia, particularly a sliding hiatal hernia, can contribute to the development of GERD. When part of the stomach pushes up through the diaphragm, it can weaken the lower esophageal sphincter (LES), which normally prevents stomach acid from flowing back into the esophagus. This weakened LES makes it easier for acid reflux to occur, leading to GERD symptoms.
From a VA disability perspective, GERD and hiatal hernia are often rated together under the same diagnostic code (7346). This is because the symptoms and health impacts of these conditions are so closely related. When filing a claim, veterans should document all symptoms related to both conditions to ensure a comprehensive evaluation.
It’s also worth noting that if a veteran’s GERD is secondary to their service-connected hiatal hernia, they may be eligible for secondary service connection. This means that even if the GERD developed after military service, it could still be considered service-connected if it’s a result of the hiatal hernia.
Secondary Conditions Linked to Hiatal Hernia
Hiatal hernias can lead to or exacerbate other health conditions, which the VA may consider as secondary conditions when evaluating a veteran’s disability claim. Recognizing these secondary conditions is crucial for veterans seeking comprehensive compensation for their service-connected disabilities. Here are some common secondary conditions linked to hiatal hernia:
1. Esophagitis: Chronic inflammation of the esophagus can result from persistent acid reflux associated with hiatal hernia.
2. Barrett’s Esophagus: This condition, where the lining of the esophagus changes, becoming more like intestinal tissue, can develop due to long-term GERD associated with hiatal hernia.
3. Respiratory Issues: Acid reflux can sometimes lead to respiratory problems, including asthma or chronic cough.
4. Sleep Apnea: There’s evidence suggesting a link between GERD (often associated with hiatal hernia) and sleep apnea.
5. Dental Problems: Chronic acid reflux can erode tooth enamel, leading to dental issues.
6. Strictures: Narrowing of the esophagus due to chronic inflammation can occur.
7. Anemia: In severe cases, chronic blood loss from esophageal erosion can lead to anemia.
8. Anxiety and Depression: Chronic pain and discomfort from hiatal hernia can contribute to mental health issues.
When filing a VA claim, it’s important to document any of these secondary conditions and provide medical evidence linking them to your service-connected hiatal hernia. This comprehensive approach can lead to a more accurate overall disability rating and ensure you receive appropriate compensation for all aspects of your condition.
Appealing a VA Rating Decision
If you receive a VA rating decision for your hiatal hernia that you believe doesn’t accurately reflect the severity of your condition, you have the right to appeal. The appeals process can be complex, but understanding your options can help you navigate it more effectively.
As of February 2019, the VA implemented a new appeals system called the Appeals Modernization Act (AMA). Under this system, veterans have three options for appealing a decision:
1. Higher-Level Review: You can request a review by a more senior VA employee. No new evidence can be submitted with this option.
2. Supplemental Claim: This option allows you to submit new and relevant evidence to support your claim.
3. Appeal to the Board of Veterans’ Appeals: You can appeal directly to the Board, with options for a direct review, submission of additional evidence, or a hearing.
When appealing a hiatal hernia rating decision, consider the following:
- Review the decision carefully to understand why your claim was denied or why you received a lower rating than expected.
- Gather any new medical evidence that supports your claim for a higher rating.
- Consider getting a medical opinion that specifically addresses how your symptoms align with the VA’s rating criteria.
- Be aware of deadlines. Generally, you have one year from the date of your decision to file an appeal.
Many veterans find it helpful to work with a Veterans Service Organization (VSO) or a VA-accredited attorney during the appeals process. These professionals can provide valuable guidance and help you present the strongest possible case for a higher rating.
Remember, persistence can pay off. If you believe your hiatal hernia is more severe than your current rating reflects, don’t hesitate to use the appeals process to seek the compensation you deserve.
Resources and Tools for Veterans with Hiatal Hernia
Veterans dealing with hiatal hernia have several resources and tools available to help them manage their condition and navigate the VA benefits system. Here are some valuable resources to consider:
1. VA Health Care: Eligible veterans can receive treatment for hiatal hernia through VA medical centers and clinics. Visit the VA Health Care website to learn more about eligibility and services.
2. eBenefits Portal: This online platform allows veterans to file claims, track their status, and access important documents. Visit eBenefits to create an account.
3. Veterans Service Organizations (VSOs): Organizations like the American Legion, Veterans of Foreign Wars (VFW), and Disabled American Veterans (DAV) offer free assistance with VA claims and appeals.
4. VA Disability Calculator: Tools like the VA.gov Disability Calculator can help you estimate your combined disability rating.
5. VA Mobile Apps: The VA offers several mobile apps that can help veterans manage their health, including the PTSD Coach and the VA Health Chat.
6. Veterans Crisis Line: For veterans experiencing mental health crises related to their condition, the Veterans Crisis Line provides 24/7 support.
7. Advocacy Groups: Organizations like the Disabled Veterans National Foundation offer resources and support for veterans with various disabilities, including digestive disorders.
Remember, knowledge is power when it comes to managing your health and securing appropriate VA benefits. Don’t hesitate to reach out to these resources for support and guidance throughout your journey with hiatal hernia.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.


















