There are a lot of different conditions that can lead to digestive issues. But some are more well-known than others (can medical issues have brand recognition?). Many types of Inflammatory Bowel Disease, for instance, are familiar to many at this point.
Compared to, say, Chron’s and Celiac, something like diverticulitis is basically unheard of—and a lot harder to pronounce. Still, those who suffer from it are dealing with a real condition, and for veterans (who are at higher risk for it), it may be impeding their ability to work or address daily responsibilities.
Thankfully, diverticulitis often qualifies for VA disability benefits. So let’s talk about what it is, how to know if you might have it, and what kind of assistance you can potentially secure if it’s service-related.
What Is Diverticulitis?
We’ll begin with some basics about the medical condition, and hallmark symptoms that patients experience.
Diverticu-What now?
Diverticulitis is a mouthful of a term that refers to inflammation of abnormal bulges in the lower intestines. That’s a bit confusing if you don’t have a few foundational pieces of medical knowledge:
- Normally, your lower intestine/colon should be smooth when healthy. Bulges inward or outward are often a sign of an underlying medical concern.
- Like many non-standard shapes that body parts can take, the pouches themselves are not the issue and don’t inherently cause problems or discomfort. But they do make certain problems more likely.
- You can have just one bulging pouch (diverticulum), or multiple (diverticula), but if you have any, it’s known as diverticulosis. It’s only classified as diverticulitis if the bulges become inflamed.
Diverticulitis is when abnormalities in colon shape develop, then become aggravated and inflamed.
You can have diverticulosis, and be completely asymptomatic, without any discomfort, or even reason to suspect you may have the medical condition. It’s only once inflammation enters the equation that it becomes painful and disruptive.
Inflammation is the body’s normal response to infection, so while infection isn’t always involved in a flare-up, every infection does lead to inflammation (and the symptoms that come with it). Because diverticula are by definition changes in the colon’s shape, it increases the likeliness of issues like tearing, accrual of fecal matter, and other issues, all of which tend to result in infections (and thus, the inflammation and flare-ups).
Diverticulitis Symptoms
What does this condition feel like, if you have it? Well, it can be acute, clearing up after a single round of treatment. Or it can be ongoing and chronic, posing long-term difficulties and increasing risks for complications. As mentioned above, you can be fully asymptomatic, you might have mild to moderate symptoms, or you may have severe symptoms and complications.
The hallmark symptoms of diverticulitis include severe abdominal pain, usually focused on a single side (the left side in particular). In fact, you may actually be able to pinpoint externally the location of the inflamed bulge due to how localized the pain is. In some cases, you can even feel the shape of your colon from the outside with your hand.
The abdominal distress can be acute, where pain onsets rapidly, with minimal warning. Or, it can gradually escalate across several days before reaching its peak. Pain can be mild, but more often is rated toward the higher end of the pain scale by patients. And it will likely feel sharp and/or burning (it is inflammation, after all).
Other than pain, you might experience a few other symptoms, all of which help pin down a diagnosis:
- Similar to abdominal pain, you may experience tenderness and sensitivity, even when the area is simply touched.
- You may notice changes in your bowel movements, like constipation or diarrhea.
- Upset stomach, nausea, and even vomiting in some cases.
- In more intense cases, patients may deal with a “distended abdomen,” meaning you can even feel your colon by hand, simply by pressing around on your abdomen.
- Rectal bleeding.
- Fever (an important one, as this is an uncommon symptom among other digestive issues).
- Increased white blood cell count (another critical diagnostic symptom, though you won’t know this one without some help from the experts).
Diagnosis and Treatment
Getting a diagnosis for this diverticulitis can be a bit of a process. It’s that way for most major issues that deal with the lower intestines. There are a lot of shared symptoms, and determining the root cause often requires going as far as making trips to the radiology department for imaging. It’s a process of elimination, striking possible culprits from the list until only the right medical condition remains.
And, as they tend to do, your doctor will likely begin with the least invasive methods first, escalating as necessary to close in on the answer.
So you’ll likely have an exam in the clinic that largely resembles a normal visit. The doctor will look over your medical records and examine your abdomen visually and with careful palpation (clinician speak for “does it hurt when I press here?”). This may lead to other approaches and tests like a pelvic exam and a pregnancy test if relevant, just to rule out non-digestive causes.
From there, you’ll probably have to do lab work. Urine samples, blood draws, and even stool tests (we are talking about the digestive tract, lest we forget). And you may be tested for liver disease.
Finally, if there’s strong medical evidence to suggest diverticulitis but it’s still inconclusive, you may be sent for a CT scan, which will clearly show the shape of your colon (and whether there are bulges or other shapes to be concerned about.
As for treatment, that will depend entirely on how severe symptoms are, and whether there may be a complication. For mild cases, you’ll likely be treated at home. You’ll be advised to make some dietary changes (possibly even put on a liquid diet until your symptoms improve) and may be given some antibiotics (to deal with the infection).
In more extreme cases, surgery may be needed to address the issue.
Regardless of severity, if problems are chronic or recurring, your doctor will likely want to monitor your disorder regularly and might recommend some long-term lifestyle and diet changes to minimize your risks moving forward.
“You Know, Diverticulitis Sounds a Lot Like…”
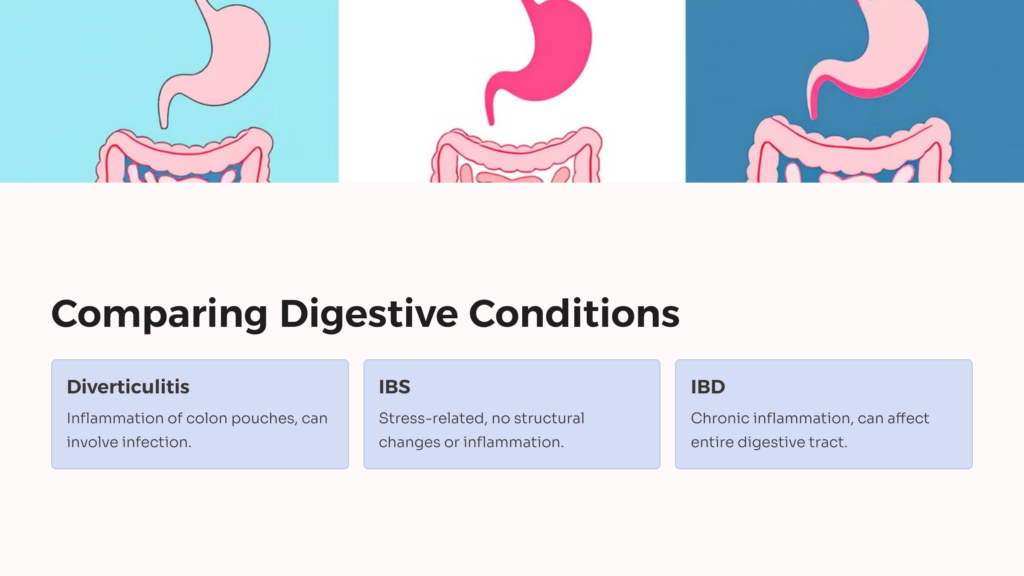
Yeah, we know. Digestive issues are like that. Here’s a very rudimentary overview of how some of these conditions compare, and what signs might point to one or the other.
Irritable Bowel Syndrome
Irritable Bowel Syndrome, or IBS, is similar to diverticulitis in how it presents—abdominal pain with inconsistent flare-ups and difficult-to-determine triggers. What makes it stand out is the mechanism underlying the pain. IBS is tied heavily to sensitivity and nerve function and can be heavily impacted by stress, anxiety, and other psychological factors.
The disorder doesn’t really have to do with the shape of the colon or digestive malfunction at all—most often, patients experience discomfort when their brain’s stress response leads to the digestive tract abruptly hitting the brakes. This technically happens to everyone (your body doesn’t want to waste energy breaking down food when running from a tiger), but IBS patients are affected more dramatically by this process.
Notably, IBS doesn’t come with fevers or a higher white blood count. There’s nothing on imaging that would flag it specifically. And it’s basically the “random bucket” where you end up when doctors can conclusively say you don’t have anything else.
Inflammatory Bowel Disease
Despite having both “inflammatory” and “disease” in the name, conditions under the IBD umbrella don’t have much to do with infection, if at all. This category (and it’s a category, not a single condition) refers to several ailments where the body struggles with some aspect of the digestive process.
Like allergies and autoimmune conditions, they’re tied to “glitches” in how your body responds to perceived threats. And while the symptoms are commonly seen in the intestines, they’re not confined there, or even to just the large intestines like diverticulitis.
Understanding Diverticulitis VA Rating
While different patients will experience different things, on the sliding scale from nuisance to grave peril, diverticulitis is between IBS (annoying, but mostly manageable) and IBD (more severe, and in some cases life-threatening).
Diverticulitis can be mild, potentially acute, and relatively easy to manage. Or it can be intense and require some pretty invasive treatment. This, as you might imagine, has a pretty direct impact on the VA disability rating of your claim.
As a standalone condition, diverticulitis can get one of three ratings:
- 0%, if you’re asymptomatic or your symptoms are mild; your condition is easily treated and/or acute; and there are no further complications connected to the diagnosis.
- 20% if you’ve been hospitalized at least once in the last twelve months for diverticulitis.
- 30% if you’ve been hospitalized at least once for the condition, and you’re dealing with some additional complication that the condition caused or is aggravating.
What’s more, diverticulitis can be awarded a rating as a secondary condition, and can be used to help calculate Total Disability based on Individual Unemployability (TDIU). It’s hard to ignore the difficulty a vet experiences if their frequent, agonizing trips to the bathroom make it a challenge to hold down jobs.
There are a lot of conditions that qualify for VA disability benefits that may seem inconsequential at first blush. But if you’re suffering as a result of your time in the service, you deserve to receive the help that the VA benefit program was established in order to provide to you. Even if the crap you’re dealing with (pardon the pun) feels less significant to you than the problems that others face.
Higher baseline levels of pain tend to become old hat as we all get older, but that’s not necessarily a good reason to ignore things that are uncomfortable. Especially if it’s making it hard to handle daily responsibilities. So don’t disregard it if your discomfort is starting to feel a little concerning. And don’t be afraid to seek help.
Not sure where to start? Then visit AllVeteran.com and take our quiz for a free medical evidence screening.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.