The United States Department of Veterans Affairs (VA), plays a vital role in the lives of the country’s military veterans. One of its significant functions is the issuance of the VA Development Letter. This article begins with a brief explanation of what a VA Development Letter is and then delves into the impact and requirements of these letters. The purpose of this article is to illuminate the importance of understanding VA Development letters.
Understanding VA Development Letter: The Basics
A VA Development Letter is an official correspondence sent out by the Veterans Affairs Department. It constitutes an essential step in the VA claim evaluation process that every veteran goes through when applying for benefits. Understanding the VA Development Letter is critical for any veteran as it allows them to navigate the VA benefits claim process more effectively.
The VA Development Letter serves several purposes and carries paramount importance. The primary reason the Department of Veterans Affairs sends out this letter is to inform veterans about the requirements and updates regarding their claim for benefits. The VA letter typically contains details about ongoing claims, aspects still under review, and any additional evidence needed a VA fully developed claim.
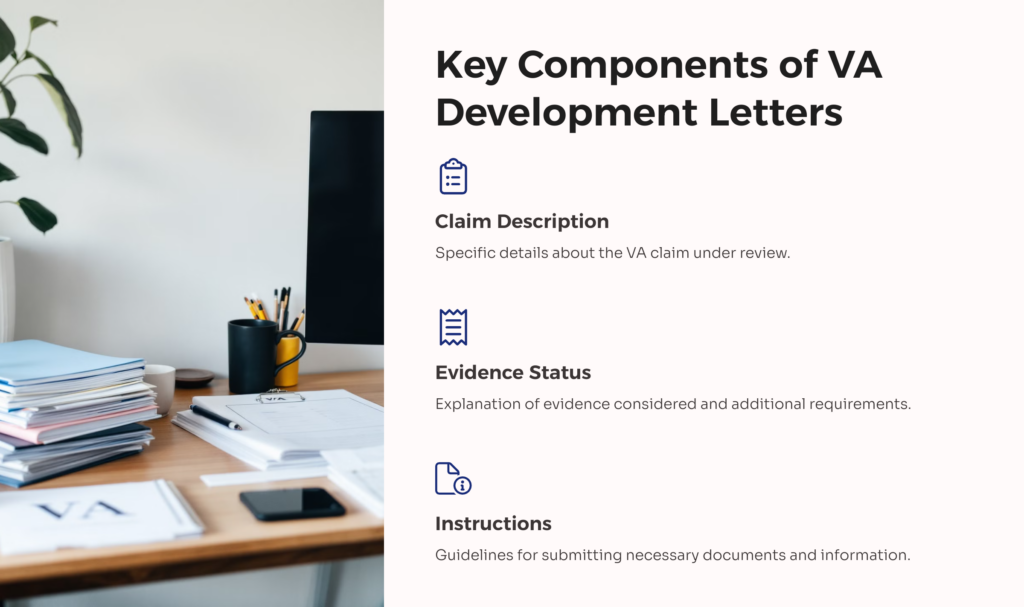
Each VA Development Letter covers the following main points:
- Description of the specific VA claim under review.
- Explanation of any evidence that has been considered thus far.
- Details about additional evidence or documentation required.
- Instructions on how and where to send necessary documents or other information.
- Timeline and rules for providing the required evidence.
The Relevance of the VA Development Letter
VA Development Letter for Claim Evaluation
The VA Development Letter aids in the process of VA disability claim evaluation by informing the veterans about the specifics of their claims. It gives a status update on the ongoing evaluations, enabling veterans to understand the progress of their claims.
VA Development Letter for Evidence Gathering
Another vital role of the VA letter is its function in evidence gathering. The VA Development Letter includes a list of necessary documentation or records needed to process the VA disability claim. It assists veterans in understanding the exact documents required, preventing any delays due to incomplete paperwork.
Process of Receiving VA Development Letter
Certain criteria warrant being sent a VA Development Letter from the Veterans Affairs. Upon submission of a claim for benefits, if there are any outstanding issues or evidence requirements, the VA will send a Development Letter to the concerned veteran.
The general time frame for receiving the VA Development Letter after applying for a VA benefit varies greatly. Typically, a veteran can expect to receive the letter within a couple of weeks to a few months after their initial benefit claim submission. The period is dependent on the VA’s workload and the complexity of the claim for VA disability benefits.
Navigating the VA Development Letter
Steps to Take After Receiving the Letter
Once a veteran receives a VA Development Letter, the first step is to read through it meticulously. Understanding the letter’s requirements is crucial. The veteran should gather the necessary documents, fulfill the requirements, and provide any additional information requested.
Properly Responding to the VA Development Letter
Responding to the requests in VA development letters should be done promptly to ensure the smooth progression of the claim evaluation. Keep copies of all communications and proofs of document submissions. In case of doubts or difficulties, consulting with a trained VA representative or VSO (Veterans Service Organization) can provide valuable advice.
Common Questions and Misunderstandings about the VA Development Letter
There are numerous misconceptions about VA development letters which can create undue stress for veterans going through the VA disability benefits claim process. One misunderstanding is around the notion that receiving a VA Development Letter signifies a denial of claims. However, this is not true as receiving a VA Development Letter is a common part of the claim process.
Amongst the frequently asked questions about the VA Development Letter, some common ones include queries about the timeline for response, repercussions of not answering the letter, and the availability of help in responding to the letter.
How VA Development Letter Affect Your VA Benefits Claim
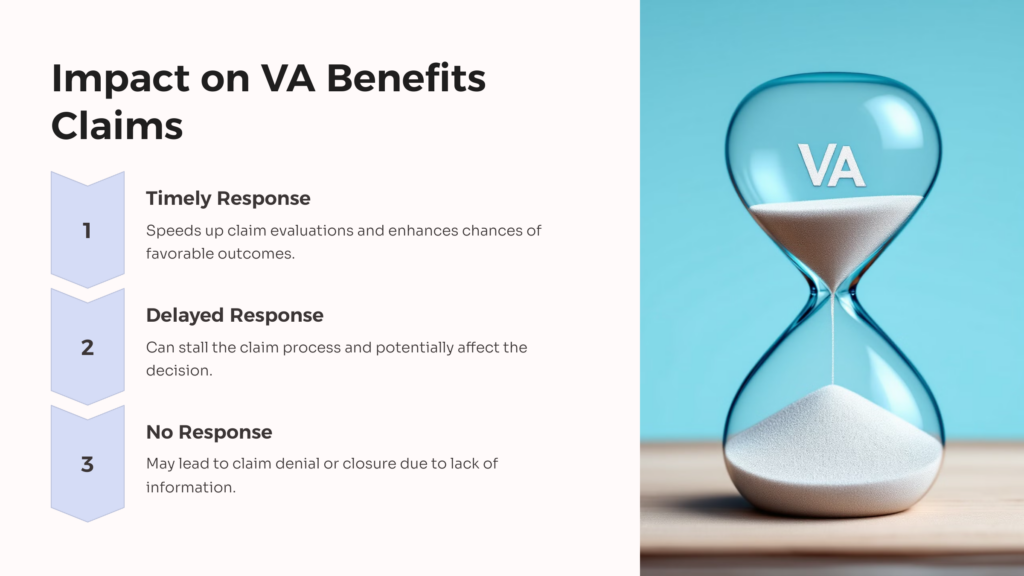
The VA Development Letter plays a significant role in the procedure of a VA benefits claim. Not responding or delaying a response to the letter can stall the claim process. Conversely, a timely and accurate response can speed up claim evaluations and enhance the chances of a favorable outcome.
Conclusion
In understanding and navigating the VA benefits claim process, the VA Development Letter is a central element. Its role in claim evaluations, evidence gathering, and communication cannot be overstated. However, while this guide offers an overall understanding, the importance of seeking legal or professional advice during the VA benefits claim process remains pertinent.
The details here aim to provide clarity about the VA Development Letter and its role. If you have further questions or would like to share your experiences with the VA Development Letter, feel free to do so. Your insights can help others navigating similar stages in their veterans’ benefits claim process.
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.