If you’re dealing with Irritable Bowel Syndrome and trying to make sense of your IBS VA rating, you’re not alone. IBS is common among veterans, and as of May 19, 2024, the VA updated the digestive rating schedule with clearer criteria for IBS under Diagnostic Code 7319. Ratings now hinge on how often you have pain related to bowel movements and how many classic IBS features you experience.
What IBS Is and Why It Hits Veterans Hard
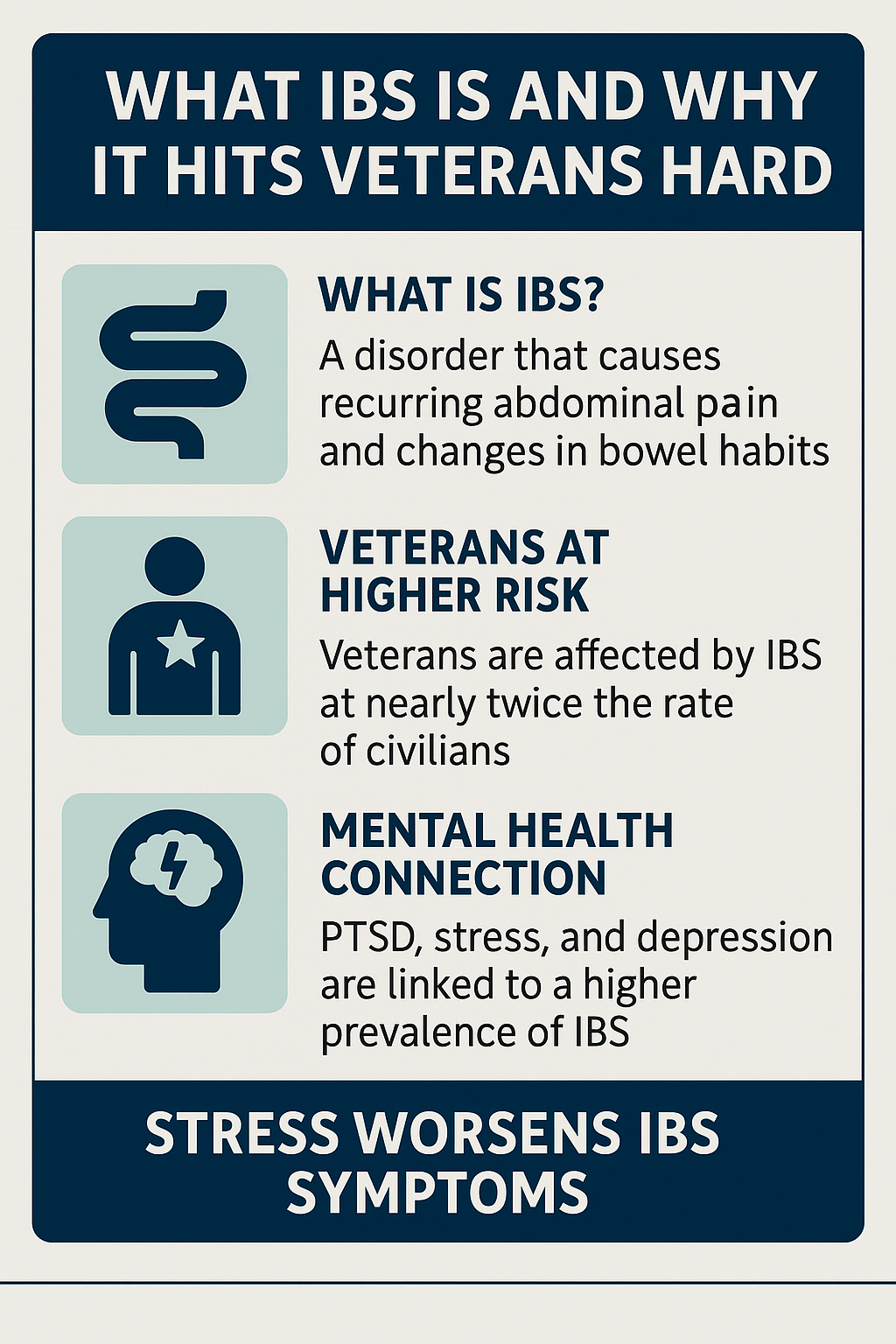
IBS is a functional gastrointestinal disorder that causes recurring abdominal pain and changes in bowel habits. It isn’t the same as inflammatory bowel disease, and it doesn’t usually show up on scans, but it can still be disruptive and exhausting. Diagnosis is clinical, often based on the Rome IV criteria.
Veterans experience IBS more often than civilians. While studies in the general population estimate around 5–15 percent of adults have IBS, surveys among veterans show nearly 30 percent meet diagnostic criteria, with higher rates among female veterans. Gulf War veterans show some of the highest prevalence rates, partly due to environmental exposures and deployment stress.
IBS and mental health conditions often overlap. Veterans with PTSD, anxiety, or depression are far more likely to develop IBS or other gastrointestinal disorders. Stress directly affects the gut–brain axis, worsening symptoms and reducing quality of life.
VA’s Current IBS Rating Criteria (Effective May 19, 2024)
IBS is rated under Diagnostic Code 7319. These are the criteria the VA currently uses:
- 30 percent
Abdominal pain related to defecation at least one day per week during the past three months, plus two or more of these symptoms: change in stool frequency, change in stool form, altered stool passage (straining or urgency), mucus in stool, abdominal bloating, or subjective distension. - 20 percent
Abdominal pain related to defecation at least three days per month during the past three months, plus two or more of the same features. - 10 percent
Abdominal pain related to defecation at least once during the past three months, plus two or more of the same features. - 0 percent
IBS that’s service connected but not compensable. You won’t receive monthly payments, but the condition is recognized, which can help with future claims.
The schedule caps IBS at 30 percent. If symptoms are severe enough to prevent substantially gainful employment, you can pursue a Total Disability Individual Unemployability (TDIU) claim for higher compensation.
The 2024 update replaced vague “mild,” “moderate,” and “severe” wording with measurable frequency and symptom criteria, making it easier to match real-world cases to the correct rating level.
How to Establish Service Connection for IBS
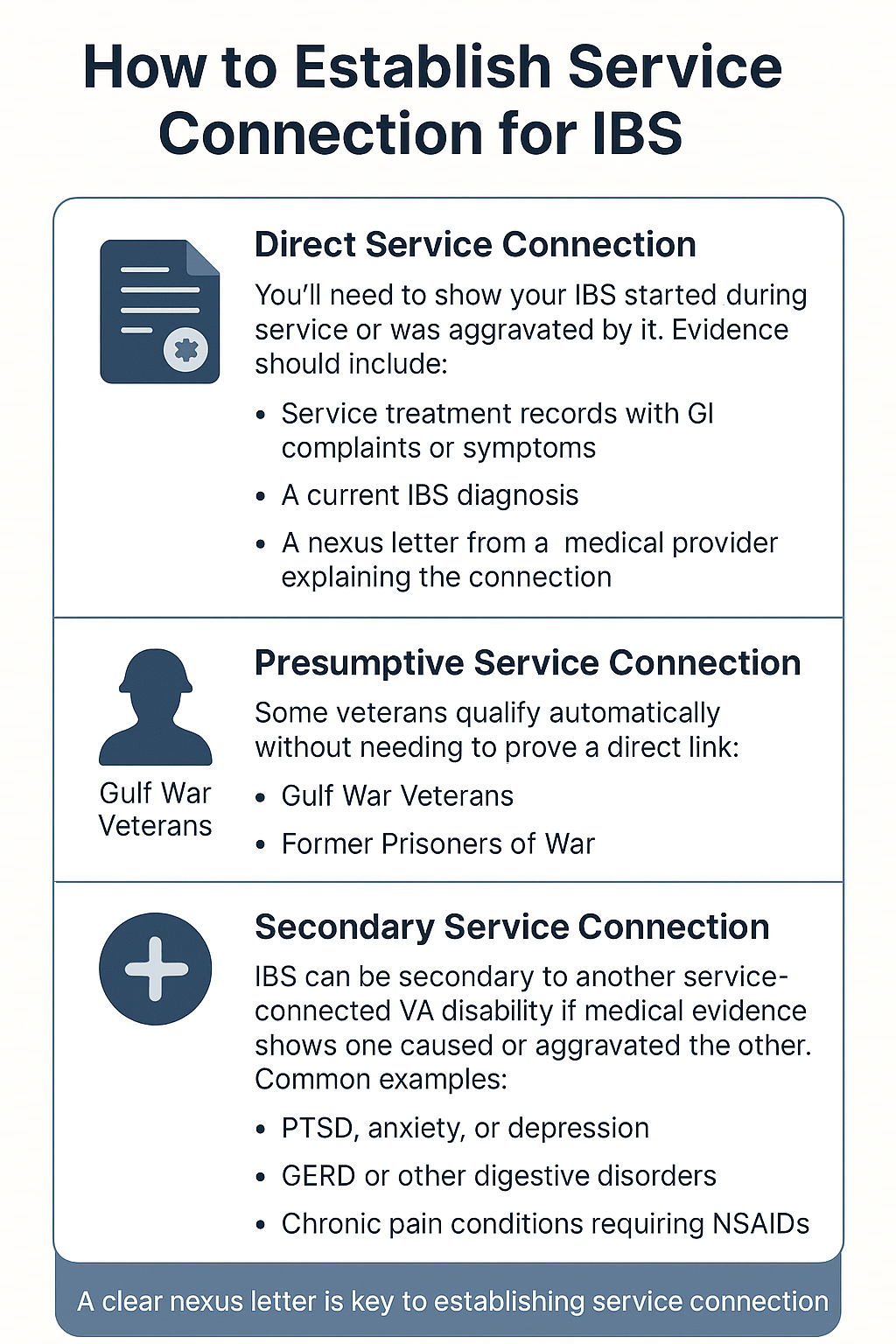
You can qualify for VA disability in three main ways:
1. Direct Service Connection
You’ll need to show your IBS started during service or was aggravated by it. Evidence should include:
- Service treatment records with GI complaints or symptoms
- A current IBS diagnosis
- A nexus letter from a medical provider explaining how your IBS is at least as likely as not connected to your military service
2. Presumptive Service Connection
Some veterans qualify automatically without needing to prove a direct link:
- Gulf War Veterans: If you served in the Southwest Asia theater since August 2, 1990, and have IBS rated at least 10 percent disabling, it’s presumed to be service-connected. IBS is classified as a “functional gastrointestinal disorder” under VA regulations.
- Former Prisoners of War: Veterans detained for at least 30 days also qualify for presumptive service connection for IBS.
3. Secondary Service Connection
IBS can be secondary to another service-connected VA disability if medical evidence shows one caused or aggravated the other. Common examples:
- PTSD, anxiety, or depression (mental health stress worsens GI symptoms)
- GERD or other digestive disorders
- Chronic pain conditions requiring NSAIDs that irritate the GI tract
A clear nexus letter is key. The provider must explain the relationship and use the phrase “at least as likely as not” to align with VA standards.
Building Strong Evidence for Your Claim
To secure the best possible IBS VA rating, you’ll need comprehensive and consistent documentation.
Key Evidence to Include
1. Medical Diagnosis
Get a formal diagnosis from a qualified medical provider. Ensure it reflects the current Rome IV criteria.
2. Medical Records
Include both service and post-service medical records that show ongoing symptoms, treatments, and any aggravations.
3. Nexus Letter
Ask your doctor to connect your IBS to service or another disability using clear medical reasoning and language that meets VA standards.
4. Disability Benefits Questionnaire (DBQ)
A completed Gastrointestinal DBQ provides detailed symptom and functional data in the VA’s preferred format. It’s one of the most efficient ways to communicate your condition’s impact.
5. Lay Evidence
Personal statements describing how IBS affects your daily life—missed work, social isolation, travel limitations—are valuable. Statements from family or fellow service members who witnessed your struggles can further strengthen your claim.
Preparing for Your C&P Exam
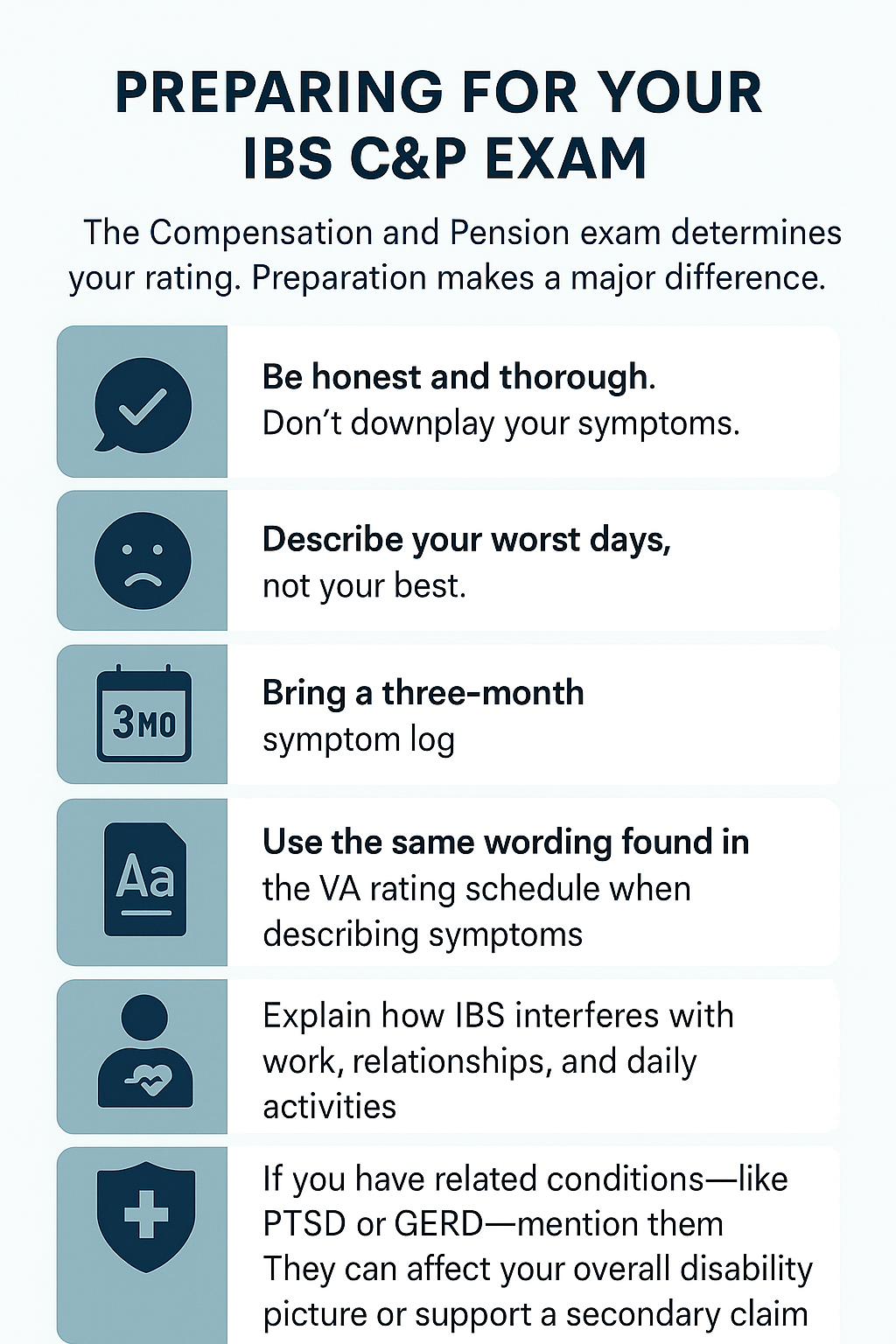
The Compensation and Pension exam determines your rating. Preparation makes a major difference.
Tips:
- Be honest and thorough. Don’t downplay your symptoms.
- Describe your worst days, not your best.
- Bring a three-month symptom log.
- Use the same wording found in the VA rating schedule when describing symptoms.
- Explain how IBS interferes with work, relationships, and daily activities.
If you have related conditions—like PTSD or GERD—mention them. They can affect your overall disability picture or support a secondary claim.
Maximizing Your IBS VA Rating
If you think your current rating doesn’t reflect the severity of your condition, you can:
- Submit updated medical evidence showing worsening symptoms
- File for a re-evaluation using the new 2024 criteria
- Request a new DBQ from your provider
- Include records of work absences or employment issues caused by IBS
- Apply for TDIU if IBS and related conditions prevent you from maintaining steady work
Appealing a Denial or Low Rating
If your claim was denied or under-rated, you have three appeal options:
- Supplemental Claim: Submit new, relevant evidence
- Higher-Level Review: Ask a senior reviewer to reassess the existing record
- Board Appeal: Have a Veterans Law Judge review your case
Common reasons for denial include missing nexus letters, unclear medical evidence, or inconsistent symptom descriptions. Fixing those issues before reapplying can significantly improve your chances.
IBS and Mental Health Connections
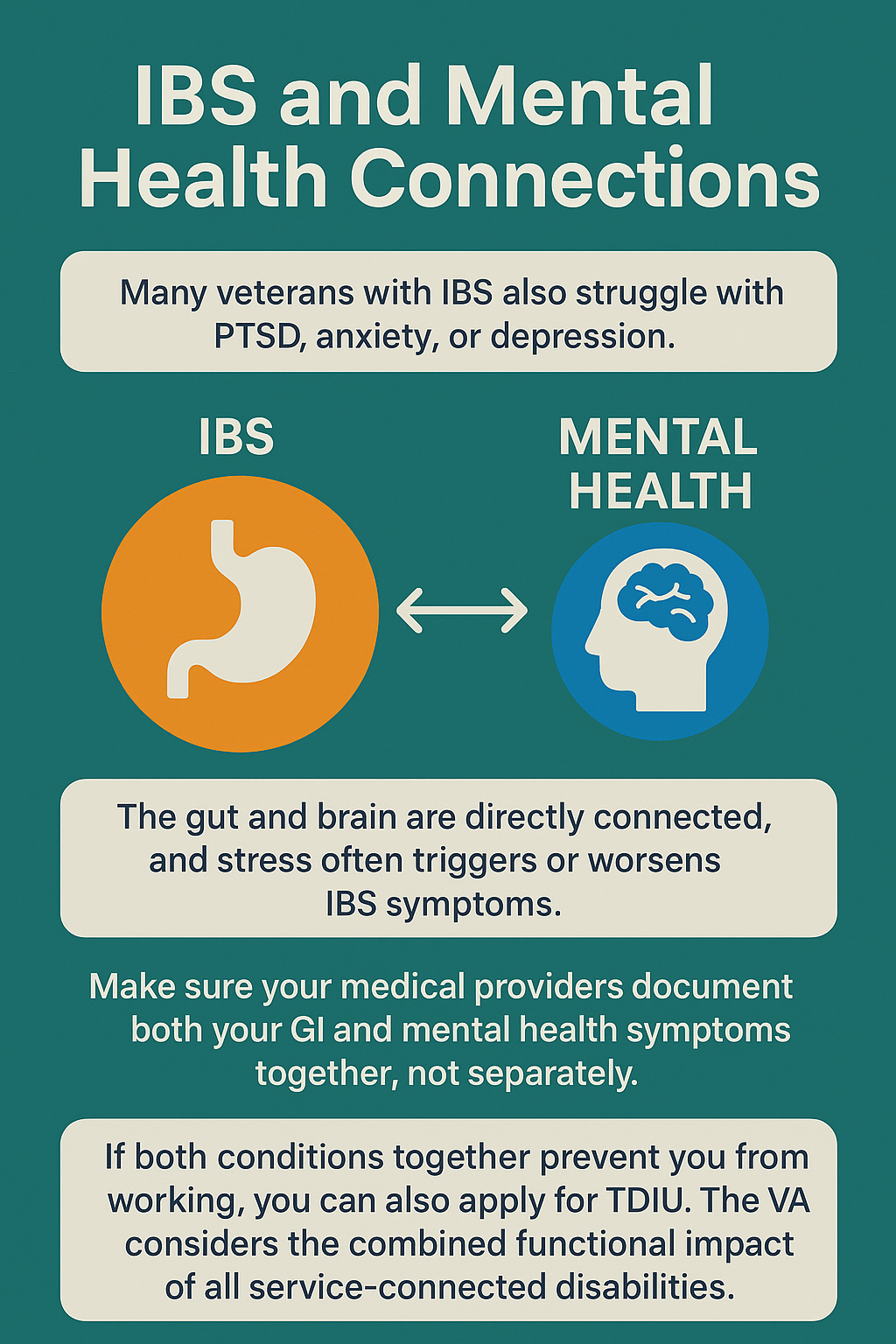
Many veterans with IBS also struggle with PTSD, anxiety, or depression. The gut and brain are directly connected, and stress often triggers or worsens IBS symptoms. Make sure your medical providers document both your GI and mental health symptoms together, not separately. This helps establish secondary service connections or higher combined ratings.
If both conditions together prevent you from working, you can also apply for TDIU. The VA considers the combined functional impact of all service-connected disabilities.
Quick FAQs
When did the new IBS criteria take effect?
May 19, 2024.
What are the rating levels for IBS?
0%, 10%, 20%, and 30%, based on symptom frequency and severity.
Can Gulf War veterans get presumptive service connection?
Yes, if you served in the Southwest Asia theater and your IBS is at least 10% disabling.
Can you get separate ratings for GERD and IBS?
Yes, if the symptoms are distinct and not overlapping (no “pyramiding”).
What’s the maximum schedular rating for IBS?
30%. However, you can pursue TDIU if IBS and related conditions prevent full-time employment.
Bottom Line
The VA’s 2024 update to the IBS rating schedule gives veterans a clearer, fairer system to match symptoms to compensation. Understanding how the IBS VA rating works—and building strong medical and personal evidence—can make the difference between a denied claim and a successful one.
If you served in the Gulf War or are a former POW, check presumptive rules—they can simplify your claim. If your IBS is connected to PTSD or other mental health conditions, document those links carefully. And if your symptoms have worsened or your current rating feels too low, gather fresh evidence and consider an appeal.
Don’t go through the process alone. Reach out to a Veterans Service Organization or an accredited representative. They can help ensure your paperwork, medical evidence, and claim strategy line up with VA standards. With persistence and the right support, you can secure an IBS VA rating that accurately reflects your condition and get the benefits you’ve earned through your service.
At Allveteran.com, we seek to help veterans connect with resources that may make all the difference. To find out your disability rating, take our free medical evidence screening today!
 AllVeteran.com Advisors
AllVeteran.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.